Remdesivir Injuries
Age: 54
Location: CA
Admitted: 08/13/2021
To: Kaiser Permanente, Santa Clara, CA
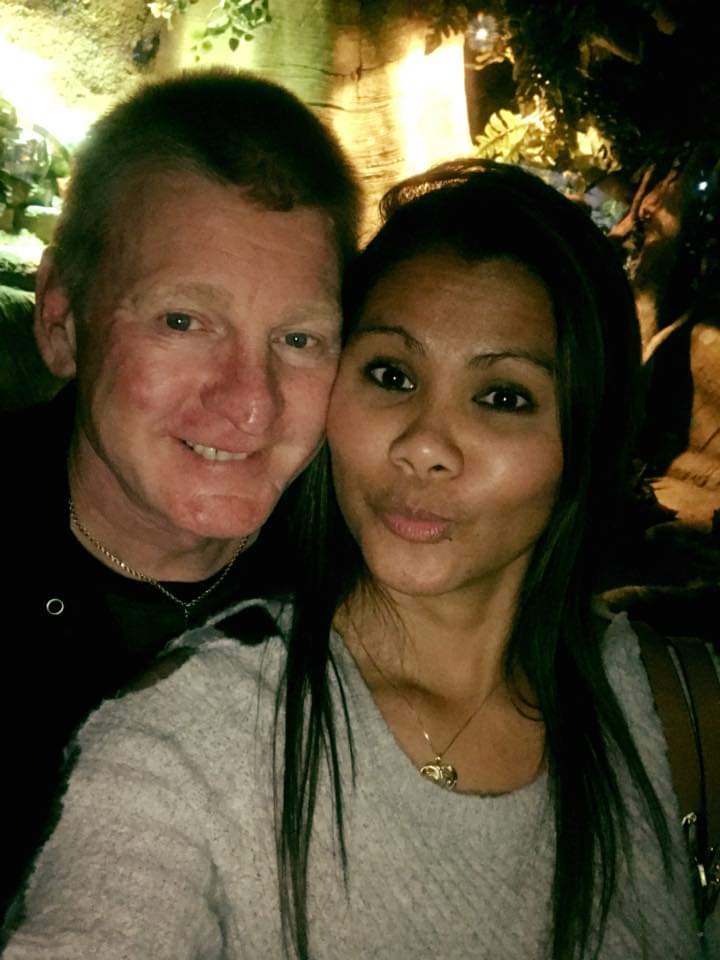
Lena Spasioti


Berated and neglected
My husband suffered a fall on 12/8/21. He suffered a suspected cervical fracture. Within 1 hour of his fall, he was placed on a ventilator.
I have been trying to move forward from the devastating loss of my sweet husband, Ron, since December 12, 2021. I continue to struggle with the circumstances and the events leading up to his death at your hospital. The appropriate care and compassion your facility DID NOT provide has made our family’s grief much more difficult to deal with.
We came to your hospital on the afternoon of Monday, November 22, 2021, because Ron was having difficulty catching his breath. We were informed by the guard, that as of that morning they were not allowing visitors. When attempting to explain to him [the guard] that my husband did not have his wallet or phone, I was informed that he was not going to argue with me, NO visitors were allowed. I was not attempting to visit, only provide Ron with the insurance cards and driver’s license that your hospital was going to need. At this point, I had not even exited my car, I had only let Ron off at the curb, and he was sitting in a wheelchair. NO ONE was arguing with the guard, we were only attempting get Ron the necessary documents. Because of the guard’s rude and totally inappropriate behavior, and his intent on enforcing a rule which no one was disputing, this was to be the last physical contact with my husband. I was not able to kiss or hug him goodbye. I could only sit in my car and wonder, was I making a huge mistake leaving him here? Come to find out, it was the biggest mistake of our lives. I wish I had taken Ron to another facility that was still allowing visitors. Not all hospitals were following the same “rules.”
After being diagnosed with COVID, he was admitted to the hospital later that evening. When I called him in his room the following morning, we discovered the room had extremely poor cell phone reception, and we were disconnected after only a few seconds. I had to ask the staff on numerous occasions to please move the hospital phone close enough for him to answer. This was the ONLY way his family was able to communicate with him. Even then it was difficult to speak to Ron because he was on oxygen, in a room with extremely noisy ventilation and laying on his stomach. I asked the staff to let us know when he was sitting up eating meals, because that was the only time he could talk. This was NEVER done. How hard would it have been to honor that small request? It certainly would have improved his mental health.
I have heard stories from numerous people, probably at more compassionate facilities, that the staff offered to do FaceTime between the patient and the family members. This was never offered to our family until Ron was on a ventilator, in a coma, waiting for the machines to be turned off. How pathetic is that, your facility could only offer this service when we were there to watch him die. At that point, it was an insult.
I was TOTALLY dependent on the hospital staff to provide me with updates on Ron’s condition. There was not a single day that they contacted me to provide an update without me having to call first and to make multiple attempts. I was told I should call at approximately 10 or 10:30 A.M., because that was after rounds. I would call EVERY DAY at that time, only to be told the nurse would have to call me back. I would wait all day for a return call. Finally, I would call again between 4 P.M. and 6 P.M. During this time, you can only imagine what my mind was thinking. To say that you people failed miserably in the communication department, is a HUGE understatement!
I can’t even allow my mind to think of the suffering Ron must have endured. I have pictures of the staffs’ attempts to start IVs and the damage that was done to his arms and hands. Then to have staff and doctors talking to him from the hallway or with protective gear and not being able to understand anything they were saying. Was any of this taken into account? Where you aware of the communication problems and just didn’t care? The isolation must have been unbearable. Because he was laying on his belly, he couldn’t watch TV, read or use electronic devices. He only had very limited communication with his family. What happens to someone’s mind during all of this? Was there any concern for the his MENTAL HEALTH? This was especially devastating, because the previous times Ron was in your hospital he had constant support from his family. It was important to both Ron and our family to be involved in his care. We were with him every step of his previous hospital stays. He NEVER would have suffered a fall if we had been allowed to assist in his care and recovery.
THEN there was the accident on 12/8/2021. Ron had been on high doses of steroids, basically immobile and eating very little for two (2) weeks. He was also, according to the physicians, suffering hallucinations. Additionally, his medical records state that he was given a new medication for anxiety that morning. Immediately after the physician’s visit, who was aware Ron was sitting on the side of the bed, he suffered a fall from his bed. Given all of these factors, why no precautions were taken to make sure that this would not happen is beyond my comprehension. Your facility was aware that he was a fall risk, and had been, from nearly the beginning of his admission. And, then to imply to me that this fall was Ron’s fault is inexcusable.
Within an hour or less of this fall, plans were being made to place Ron on a ventilator. I was contacted approximately an hour after the fall to give permission to place Ron on a ventilator. At that time, I was not allowed to speak to Ron, determine his wishes, or even to hear his voice for the last time. If your facility cannot acknowledge that this fall SEVERELY impacted his condition, then you are not being honest. It was noted in Ron’s medical records, by one of your physicians, “I suspect (condition) worsened on the basis that a c-collar is in place after a fall and clearly is not tolerating BiPAP well enough to be able to adequately clear secretion.”
Ron was immediately moved to the ICU after the fall. I wish I could say that the ICU staff was an improvement, but things only continued to decline. I was told by Ron’s primary care physician (PCP), that he was putting orders in place for me to visit Ron since there had been a significant change in his condition. That was at approximately 10 A.M. I was told that I would be contacted by someone at the hospital when this was approved. After waiting until 5:45 P.M., I called the hospital. I was told that I could come into the hospital and speak to the doctors, and see Ron through the window.
During this “window” visit I discovered that Ron’s hands were tied down. I was told this was because he had fought so hard not to go on the vent. Was he asked about going on the vent, and he said no? Was I not told this? Was I forced to make a decision against his wishes? I still have nightmares and guilt about that decision.
At this time I just wanted to touch him. I was hopeful he would still have been aware enough to know I was there. Was that too much to ask? I’m not sure why I still was not allowed to go into his room. I had COVID two (2) weeks prior, and been testing negative for some time. According to all protocol, I was safe and no risk to others. Again, just another example of the hospital’s total disregard for the patient and family. It wasn’t about doing the right thing, but enforcing a rule. One that was not even being done at other hospitals.
The following day on the 9th, I spoke to the hospital staff at 8:45 A.M. They told me Ron was holding steady, and they were going to attempt to cut back on sedation and vent support. I asked to be called when this was done and to be told how he tolerated the changes. No one called, so at 6 P.M., I called and was told the nursing staff would call me back. At 9:10 P.M., they FINALLY called me back. Asking the staff to make a 5 minute call was a reasonable request given the fact that we were denied access to Ron, and he was in the ICU on a ventilator. This lack of communication, making our family wait for over 12 hours to hear any news on our loved one is inexcusable. Again, you can only imagine what thoughts were going through our minds. Communication should have been a normal part of compassionate care.
On the 10th, I called at 8:30 A.M., and was told the nurses would call back about 10:30 A.M., after rounds. At 2:15 P.M., I was finally called back. He was stable. That was good news.
In the early morning hours of the 11th, I was contacted by the hospital. Ron was stable but not improving. They were going to allow a visit. At that time, I contacted Ron’s only daughter, Mandi, who lived over an hour away, to come to the hospital. When I got there, I met with one of the doctors on staff in the ICU. She informed me that Ron was stable, and that I could go into his room and see him. I told her that I had called his daughter and she was coming also. This was the first I heard that I was the only one who could visit. The doctor told me the only way Mandi could come see her dad was if I agreed to turn off the ventilator! Where the hell did that come from? He was stable! To say I was shocked is an understatement. I asked why she would even suggested that. She told me, while we were standing in the middle of a hall, that they were not sure how much damage had been done as the result of the fall. He could be paralyzed or have brain damage! Why was this the FIRST time I was hearing any of this? Now it was even more important that Mandi be allowed to visit her dad.
Mandi had also had Covid three (3) weeks prior and was now testing negative. Again, according to all protocol she was safe to visit. I tried to explain all this and tell them that I would leave, and she could come in my place. She had just driven over an hour in the middle of the night to see her DAD. Their response, THEY CALLED SECURITY.
I was just hit with the shock of my life. I was told by the most insensitive doctor, that my husband might be paralyzed or have brain damage, and the response was to call security? I was of no threat; I couldn’t even stand. They had brought me a chair because I was going to pass out, and they didn’t want ME to FALL. I have NEVER in my life experienced such an overwhelming lack of compassion and at such an emotionally devastating and traumatic time. The outcome was Mandi was NOT allowed to visit her dad, but come into the ER and speak to a doctor. The hospital followed their RULE, but at what cost to our family?
The following morning on the 12th, at approximately 11 A.M., we were both allowed to visit. Ron’s body was shutting down. It was at this time the decision was made to let Ron go peacefully. FINALLY, we were apparently an acceptable risk. The only people who showed ANY compassion, was the ICU nurse and respiratory therapist who stood with us as we watched Ron, our beloved HUSBAND, DAD and PAPA, take his last breath. No, we were never allowed to say goodbye when he might have understood us, because of your hospital rules.
When Ron was diagnosed with COVID we asked about specific treatment and what alternatives where available. We were told that there was only ONE acceptable protocol and that nothing else would be considered. Well, we ALL know now, BEYOND ANY DOUBT, that your protocol DID NOT WORK. RON IS DEAD. We’ll never know if something else might have been better. Again, hospital rules.
Even after Ron had passed, your hospital continued to display your lack of compassion and disregard for our family. The funeral home attempted to pick up his body and the hospital would not release it. Your hospital contacted me for three (3) days asking if I was going to have an autopsy performed. Why was this such a huge concern of yours? Is this normal, or only done if a person suffers an accident in your hospital? I had absolutely NO intention of allowing your facility to TOUCH him! It didn’t matter if I was going to have an autopsy, I had signed papers with the funeral home to release his body, and you had no legal right to hold onto him. It wasn’t until I demanded to talk to the president of your facility that you finally released his body late Wednesday afternoon. Do you even understand the additional stress and trauma you added to an already grieving family? We had a funeral planned for Friday and we were fighting to get him to the funeral home by then. I’m not sure if this was another one of your rules, or just another way to torture a grieving family. But either way, it was totally DEPLORABLE behavior.
There are no words to describe the extreme distress and heartache you have cause my family. I would hope that no other family suffered this offensive treatment, but I’m sure that is not the case. From the moment I dropped my husband at your ER doors to the time of his funeral, it was clear that you had no concern of the impact that your “rules” or behavior would have on your patients or families. I hope no one you love ever has to suffer the way we did.
I question if your informed hospital has read the studies that show there is NO proof that the strict visiting rules you enforced, even when a loved one was dying, had any impact on stopping the spread of Covid in hospitals. BUT there are numerous studies showing the extreme long term damage and hardship that you caused grieving families by your total lack of compassion and RULES.
It’s unfortunate that you choose to run this hospital as just a business, because a hospital should be so much more than that. Your BUSINESS probably cost my husband his life and our family unbearable pain and loss. If you had only displayed more compassion. If you had even offered the simplest apology for an injury that never should have occurred. We can continue to justify this behavior as the result of a pandemic, but we are all still humans that deserve to be treated as such. In that regard your hospital failed miserably.
Filter By Category
Age: 54
Location: CA
Admitted: 08/13/2021
To: Kaiser Permanente, Santa Clara, CA
Lena Spasioti

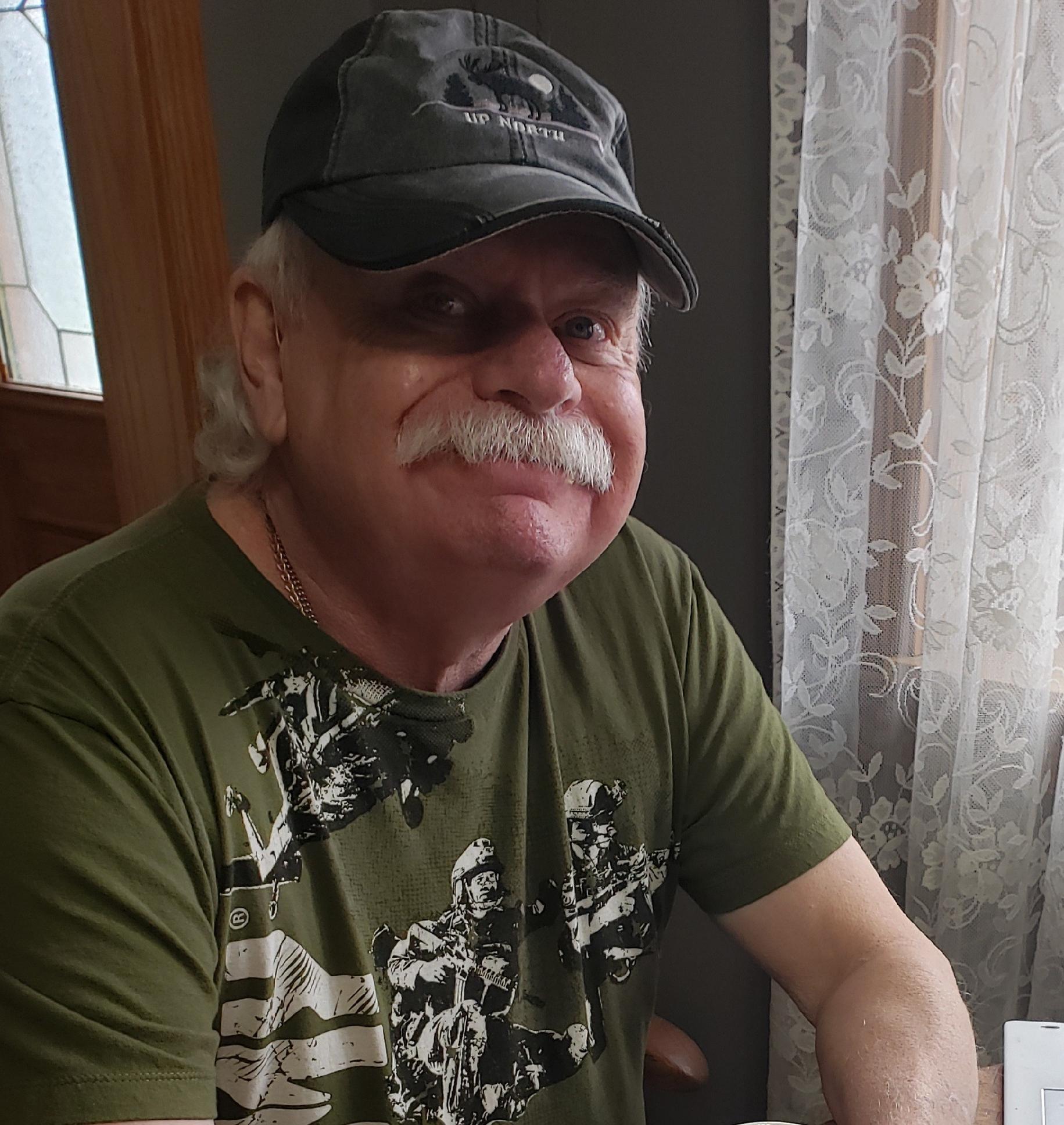
Age: 62
Location: AK
Admitted: 09/09/2021
To: Mat Su Regional
Kevin Hite

Location: PA
Admitted: 09/01/2021
To: St Lukes Fountain Hill Bethlehem, Pa
Murdered: 09/13/2021
Christopher F. Loncaric
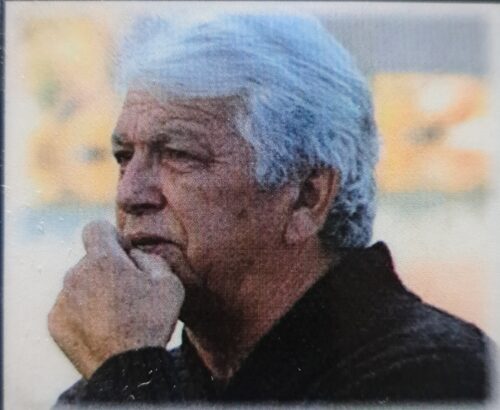
Age: 70
Location: CA
Admitted: 10/11/2021
To: Bakersfield Heart Hospital
Murdered: 10/26/2021
James Jackson, III (Sonny)

Age: 62
Location: TX
Admitted: 08/11/2021
To: Good Shepherd Hospital
Murdered: 08/26/2021
Larry Randall Wyatt

Age: 69
Location: VA
Admitted: 10/06/2021
To: Santara Martha Jefferson
Murdered: 10/20/2021
Sherman Herritt

Age: 51
Location: SC
Admitted: 09/06/2021
To: MUSC, Scouth Carolina
Murdered: 09/21/2021
Ian Bonnet

Age: 52
Location: KY
Admitted: 01/12/2021
To: Jennie Stuart Medical Center
Debra Jones

Age: 59
Location: AZ
Admitted: 11/08/2021
To: Banner Del E. Webb medical center
Murdered: 12/07/2021
Miguel Rodriguez

Age: 55
Location: NV
Admitted: 08/30/2021
To: Centennial Hills Hospital
Murdered: 09/23/2021
Ricardo Fimbres

Age: 55
Location: NC
Admitted: 11/03/2021
To: CaroMont Hospital
Murdered: 11/29/2021
Rodger C Haas

Age: 82
Location: FL
Admitted: 08/11/2021
To: The Villages Hospital -the Villages Fl
Murdered: 08/28/2021
John J Murphy Sr.

Age: 46
Location: FL
Admitted: 08/06/2021
To: Viera Hospital
Murdered: 09/09/2022
Jennifer Lynn Hubert

Age: 57
Location: FL
Admitted: 08/24/2021
To: Sarasota Memorial
Murdered: 09/14/2021
Eric Schrock

Age: 22
Location: GA
Admitted: 09/20/2021
To: Piedmont East Side Medical (Snellville)
Murdered: 09/25/2021
Jacob William Kurasaka
Age: 71
Location: MI
Admitted: 10/04/2021
To: Trinity Health Muskegon
Murdered: 10/14/2021
Douglas Niles Wilson

Age: 72
Location: MA
Admitted: 12/19/2021
To: Winchester Hospital
Murdered: 01/06/2021
Karen Jeanne Ward

Age: 66
Location: MT
Admitted: 10/24/2021
To: Logan Health Kalispell and Whitefish
Murdered: 11/02/2021
William Rowson

Age: 84
Location: PA
Admitted: 12/26/2020
To: Holy Redeemer Hospital
Murdered: 01/11/2021
Margaret(Peg) Rybas

Age: 76
Location: PA
Admitted: 12/14/2020
To: Jefferson Hospital
Murdered: 12/23/2020
Fredrick (Rick) Dodds

Age: 49
Location: GA
Admitted: 09/27/2021
To: Tanner Medical Carrollton
Stephanie Herren
Age: 40
Location: MO
Admitted: 12/31/2021
To: Mercy Joplin mo
Murdered: 01/08/2022
Merdalyn (Lyn) Greathouse

Age: 60
Location: FL
Admitted: 08/17/2021
To: St. Joseph's South
Murdered: 09/02/2021
Patricia Green

Age: 79
Location: NV
Admitted: 10/23/2022
To: Centennial Hospital, Las Vegas, NV
Murdered: 11/05/2022
Marsha Morris
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.