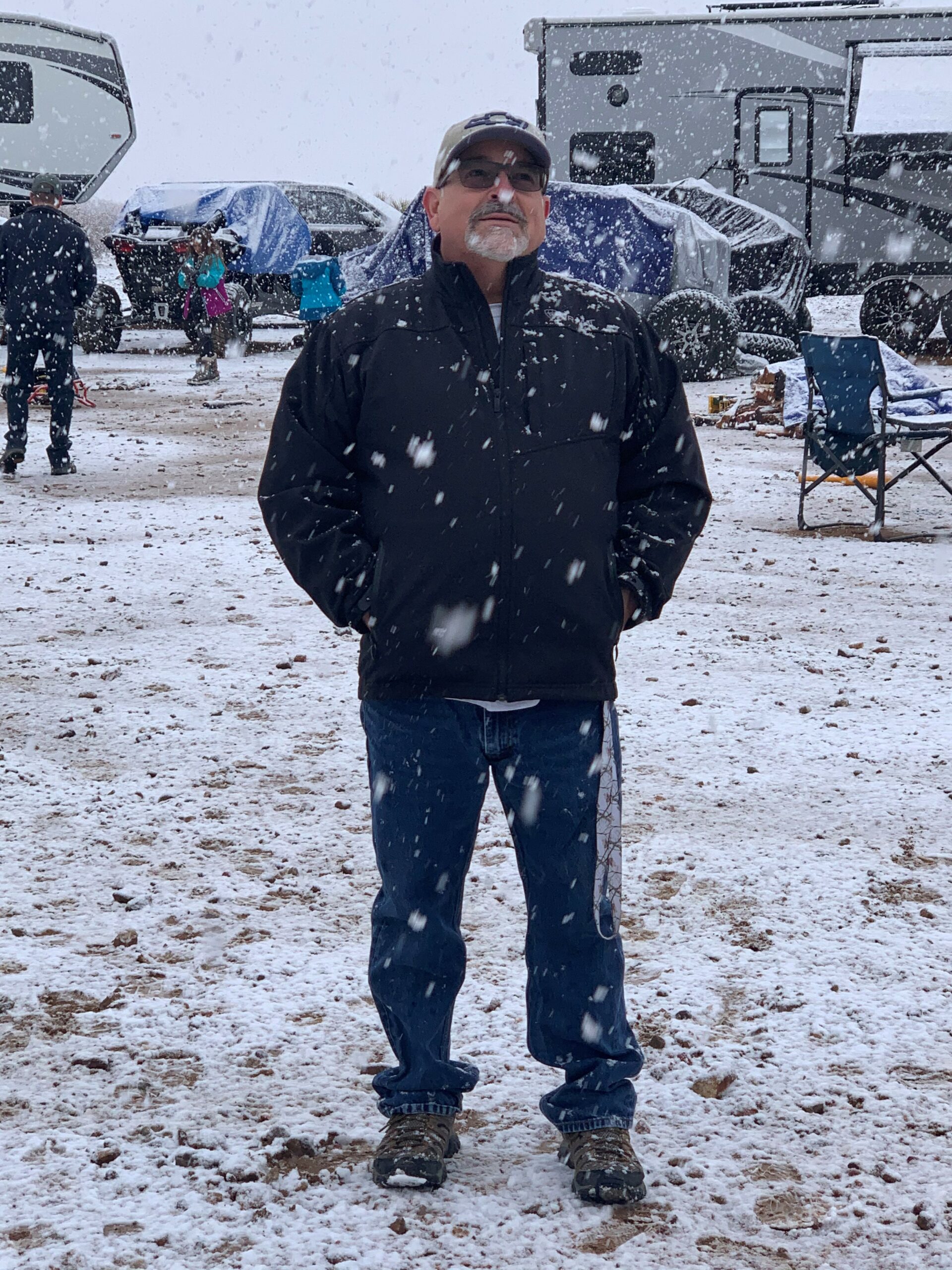
My Daddy
Age: 81
Location: NM
Admitted: 11/07/2020
To: Holy Cross Hospital
Murdered: 11/20/2020
SwiftDeer Tony B Martinez


• Sherri was left in a cold ER room with no attention for hours after her initial admittance
• She was on a bed alarm, dependent on a nurse to help her to the bathroom. After several calls to the nurse, Sherri soiled her bed and was lying for hours in her own excrement.
• She was neglected for an unreasonable amount of time for her basic needs: water, meal menus, help into the bathroom
• When asked about water for Sherri, the nurse pointed to the corner of the room and said, “it’s over there,” on a table out of the reach of Sherri who was unable to move from her bed
• Sherri had been in the hospital for pneumonia earlier in the year and was treated successfully. However, now that she had covid-19 symptoms, the hospital did not offer alternative treatments to Sherri’s conditions that would be acceptable to her
• Sherri was not allowed to take the medications that she brought to the hospital from home. These medications were shown to reduce covid symptoms when taken soon after the initial start of symptoms
• Basic needs of her visitors were not offered or provided: no water, no food, no use of bathroom facilities, can’t leave the room and return (although the nurses enter and leave, and use the bathroom). They were told not to use the bathroom facilities in the room during their 12-hour visit, and if they left the room to use a bathroom outside of the room, they would not be allowed return to the room. If they left, they had to leave the hospital without the option of a second visit.
Sherri had a sufficient supply of Ivermectin, Hydroxychloroquine and aspirin for her treatment against covid-19 but was refused from taking by Hospital staff.
My wife Sherri had breathing difficulties and was administered to Delnor Hospital in Geneva, IL on November 19 via ambulance. I put in Sherri’s purse her own medication as they took her to the hospital. I gave her:
Ivermectin 12 mg, 2 daily for 5 Days, then 2x weekly
Hydroxychloroquine, 1 daily for 12 days
Aspirin, pure 44/157, 2 daily up to 650 every 4-6 hours to prevent blood clots
Delnor Hospital refused to let Sherri take her own medication despite us pleading the case. After a few days in ER care her breathing situation got worse and she was transferred to the ICU department where she died on November 30 due to respiratory failure as a result of Covid pneumonia.
If Delnor Hospital would have let Sherri take her own medication she might be still alive. My wife complained bitterly that she was lying in a cold ER Room for six hours without anybody attending to her after initial admission. Asking for a glass of water would take 45 minutes. She finally was moved to a room that night but the care didn’t improve much.
She was laying in her own excrement for hours before someone came to change her. As days went on Sherri felt frustrated and eventually gave up and wanted to go home to be with Jesus.
I was prevented to see or be with her until the last day on Nov 30th at 11:00AM. I held her hands and comforted Sherri for 12 hours at her bedside while close friend Janet was using oils to massage Sherri’s arms and legs. It was agonizing to see my beloved Sherri struggling until her last breath at 11:37PM. If she needed more Morphium to ease the pain it would take up to 45-60 minutes before a Nurse came back. The same for a glass of water for Janet and me in the room with my wife. Janet needed to use the toilet but was told there was none in the room and if she went outside of the room she couldn’t come back in. Janet then looked around in the room and found a disguise toiled in our room.
There a plentiful examples of how the above medication could have helped Sherri including President Trump who took it.
In May, a DuPage County judge ordered Elmhurst Hospital in Elmhurst to give a doctor admitting privileges and let him give a 68-year-old woman ivermectin. She has recovered.
In November, another DuPage judge ordered Edward Hospital in Naperville to give admitting privileges to a doctor and allow him to give Ivermectin to a 71-year-old man. He has recovered.
An appellate court has refused to make an Elgin hospital give the Ivermectin to a COVID-19 patient as a treatment. The 2nd District Appellate Court ruled that Amita Health St. Joseph Hospital does not have to let Sebastian Abbinanti’s doctor give the 40-year-old man the drug.
Abbinanti and his wife, Maria, were hospitalized in late November. Their health care agents asked a Kane County judge on Dec. 15 to overrule the hospital. On Dec. 17, Judge Robert Villa refused to do so. Maria died on Dec. 21. According to social media posts, Sebastian Abbinanti remains in the hospital.
“The facts underlying this case are sad indeed,” Justice Mary Schostok wrote in the opinion issued by the three-judge appellate panel. But patients do not have a contractual right to force a hospital to give or allow a treatment not approved by the hospital, the panel ruled.
The judges didn’t rule on the merits of ivermectin. “This court is highly sympathetic to the plaintiffs’ worthy goal, which is to pursue every possible avenue that could benefit the Abbinantis’ health. However, as an appeals court in a sister state has observed, ‘judges are not doctors’ and ‘cannot practice medicine from the bench,'” Schostok wrote.
In September, the company that owns St. Joseph prohibited using oral ivermectin as a COVID-19 treatment. The drug is used to treat some parasitic conditions in humans. Federal authorities have not approved it as a treatment for COVID-19 and urge doctors not to use it off-label.
The St. Joseph case differed in that Dr. Sergei Lipov had hospital admitting privileges. The Abbinanti suit contends the hospital unlawfully interfered with Lipov’s ability to treat his patients as he saw fit. But because he is not a party to the lawsuit, Villa and the appellate judges said that didn’t apply. Both Villa and the appellate court said Abbinanti does not have a protectable right and that he is not likely to win a lawsuit.
I am very sad as I believe my wife could have had a chance to get better if she were allowed to take her own medication. By refusing her that right Delnor Hospital acted as Judge, Jury and Executioners.
Information for a Formal Complaint about the Care for Sherri Ronstadt by Northwestern Medicine Delnor Hospital, Geneva, IL
Sherri Ronstadt’s care at Northwestern Medicine Delnor Hospital, Geneva, IL from November 19 through November 30, 2021.
Here are some of the lack of medical treatment and personal care provided by the hospital:
We are aware of the following that may interfere with hospitals’ ability to make decisions centered on the care and treatment of patients with covid:
Sherri had a sufficient supply of Ivermectin, Hydroxychloroquine and aspirin for her treatment against covid-19.
This narrative is mainly anecdotal information from Sherri’s husband Rolf and her best friend Janet Kruse. Sherri kept in communication with them by phone and text messages.
It’s an approximate sequence by date. I combined Rolf’s narrative with Janet’s recounting into a daily narrative.
Background
Sherri had a history of asthma and breathing problems. She had been treated earlier in 2021 for pneumonia. Sherri has a deep Christian faith, which she lived out every day. She strongly believed that abortion is morally wrong and applied her belief to all vaccines and medications that use cells from fetal body parts or other unnatural components in its manufacture or testing.
Day -2 – Wed., November 17
Sherri flew home from visiting friends in Delaware (Nov. 14 to Nov. 17). She had dinner with friends and stayed up late telling her husband Rolf all about the trip.
Day -1 – THU., November 18
Sherri attended a dance class and showed no symptoms or problems.
Day 1 – Fri., November 19
Sherri got up in the morning and told Rolf that she didn’t feel well and couldn’t breathe. Rolf said she was pale from lack of oxygen. He ordered an ambulance, which took her to Northwestern Medicine Delnor Hospital in Elgin.
Rolf sent a supply of Ivermectin, Hydroxychloroquine, and aspirin with Sherri in her purse.
Sherri was admitted into an ER isolation room, on oxygen, and tethered to the bed with a bed alarm. If she needed to get up from the bed, she had to call the nurse. She soiled her bed and lay for hours in a dirty bed. She was left in a cold ER room for 6 hours with no attention since her initial admission. She was very cold. Asking for a glass of water took 45 minutes.
Day 2 – Sat., November 20 to Possibly Sun., November 22
Sherri was still in the ER room. On November 20, Sherri had an x-ray of the upper digestive tract with double contrast.
Day 4 – Mon., November 22 to possibly Day 8 – Fri., November 26
Sometime during these days, we believe that Sherri was moved out of the ER to a larger room. She could move to the bathroom by herself.
She felt fine, not on oxygen at this time and no longer in critical condition. Sherri was very angry, bored, lonely, and sounded normal.
She reported to Janet that she was “under observation” for a “marker” in her lungs, so she was not able to leave the hospital. No visitors were allowed.
Sherri would have to ask every morning for a menu, which took up to 45 minutes. Then wait for a nurse to pick up her order, and the order to be delivered. Most hospitals these days voluntarily deliver a menu to the rooms, or leave one from the last meal of the day.
Day 9 – Sat., November 27
Rolf received a call from the hospital saying that Sherri had taken a turn for the worst. Rolf contacted several of Sherri’s friends. The hospital gave Sherri 3 options:
The hospital offered Sherri the Remdesivir treatment and she refused it, as well as the intubation. After calling Rolf and talking about the choices, she decided on hospice because the other 2 options were not acceptable to her. Also, it was the only choice that offered the chance to have visitors to her room.
Janet called the hospital for information and they said the only option was “comfort care” (aka hospice).
One of Sherri’s friends contacted a service for a Patient Advocate to assist with communication and care on behalf of Sherri’s family and friends from outside of the hospital’s assigned doctor and nurses.
Either on Saturday or Sunday, Sherri needed an increase in oxygen and the hospital offered and tried the BPAP oxygen system and other respiratory methods that required a mask, which Sherri could not tolerate. Sherri resisted the masks on her face and declined continuing these methods.
Day 10 – Sun., November 28
The Patient Advocate, Patricia Freeman RN, set up a phone call with Sherri, Rolf and Janet. Sherri said, “They are not taking good care of me.”
Pat Freeman asked the doctor/nurse to administer Budesonide. They agreed, but we don’t know when or if it was administered.
Day 11 – Mon., November 29
Pat Freeman set up a phone call with Sherri, Rolf and Janet.
Janet was on the phone with Sherri and heard her ask the nurse for the Ivermectin and the nurse refused.
Day 12 – Tues., November 30
Sherri was given 3 options by the hospital: Remdesivir, intubation or comfort care. With comfort care, she could finally have 2 visitors. She chose the comfort care. It is inconceivable that a hospital as only these treatments for her condition—doctors are supposed to try all avenues, even off-label and trial use drugs.
Rolf and Janet arrive at the hospital at 10:30 am, are admitted at about 11:30 am. Sherri was in the ICU unit, one that has a vestibule entry. Both gowned, masked, and gloved up before entering.
During the day, Janet wanted to lower the oxygen level that was being given to Sherri from 70 units to a lower percentage. The nurse said that the higher oxygen level makes her more comfortable. Later, a nurse came in to lower the oxygen level at the time when she was setting up the morphine drip. If the lower oxygen would make Sherri less comfortable, why would she lower it?
When Janet asked for water for Sherri, the nurse waived to the corner behind Sherri’s head and said the water is over there. Sherri would not be able to reach the water from the bed.
Rolf and Janet had no water, no food, and no toilet for about 11 hours. They were not allowed to leave the room to eat and then return; once they left, they could not return to the room. They were not offered water or food or a toilet. Eventually Janet found a toilet hidden in the room, after almost 11 hours there. The hospital’s primary purpose is to provide health care and yet it could not provide basic personal needs for visitors who were there to care for their loved one?
Thank you and be abundantly blessed,
Rolf Ronstadt
630-327-0270
Filter By Category
Age: 81
Location: NM
Admitted: 11/07/2020
To: Holy Cross Hospital
Murdered: 11/20/2020
SwiftDeer Tony B Martinez

Age: 43
Location: AL
Admitted: 09/02/2021
To: Northside guntersville al
Murdered: 09/23/2021
Shannon Marie Jordan McDonald

Age: 64
Location: FL
Admitted: 07/08/2021
To: Blake Medical Center
Joseph Leo

Age: 68
Location: TN
Admitted: 11/10/2021
To: Hardin County Medical Center
Murdered: 11/15/2021
Charlotte Ulmer

Age: 83
Location: ME
Admitted: 04/13/2021
To: Northern Light - Mercy Hospital
Murdered: 04/23/2021
Judie D. Valle

Age: 61
Location: OH
Admitted: 09/13/2021
To: Genesis hospital
Murdered: 10/02/2021
William Darrell Lyons

Age: 60
Location: MO
Admitted: 09/11/2020
To: Capital Region Medical Center
Murdered: 10/06/2020
Bob Belknap

Age: 66
Location: CT
Admitted: 01/16/2022
To: Hartford Hospital
Michael Paquette Sr.
Age: 71
Location: TX
Admitted: 10/13/2021
To: Santa Christus Hospital
Murdered: 10/30/2021
Alan M. Haines

Age: 72
Location: WA
Admitted: 01/01/2022
To: PeaceHealth Southwest hospital
Murdered: 01/24/2022
Wendy Gene Nickelson

Age: 56
Location: CO
Admitted: 11/15/2021
To: North Suburban Medical Center
Murdered: 11/30/2021
Donald Russell, Jr.

Age: 79
Location: NV
Admitted: 10/23/2022
To: Centennial Hospital, Las Vegas, NV
Murdered: 11/05/2022
Marsha Morris

Age: 74
Location: VA
Admitted: 11/10/2021
To: Lewis Gale Montgomery Hospital
Murdered: 11/16/2021
Frank Ruffner Moseley

Age: 53
Location: MI
Admitted: 08/30/2021
To: Ascension Genesys Hospital
Murdered: 09/12/2021
Jonathon Goscinski

Age: 80
Location: PA
Admitted: 12/28/2021
To: Phoenixville Hospital
Murdered: 01/04/2022
Eva Hicks

Age: 56
Location: ID
Admitted: 08/26/2020
To: St Alphonsus Med Ctr
Nurse Patti Gilliano
Age: 58
Location: WI
Admitted: 09/19/2021
To: Door County Medical Center
Brenda-Lee Malley

Age: 53
Location: OR
Admitted: 09/22/2021
To: Legacy Meridian
Murdered: 10/05/2021
Greg Eyerly
Age: 59
Location: CA
Admitted: 11/09/2021
To: San Dimas Community
Murdered: 11/20/2021
Mathew Simpkins

Age: 87
Location: CA
Admitted: 12/12/2020
To: San Gorgonio Memorial Hospital Banning CA
Murdered: 12/27/2020
Barbara Ann Roberts

Age: 41
Location: MI
Matthew Webster

Age: 51
Location: KY
Admitted: 07/17/2021
To: St Elizabeth Florence, KY
Murdered: 07/26/2021
David Smith

Age: 74
Location: IL
Admitted: 11/27/2021
To: Payless
Murdered: 12/26/2021
Tom Cunningham

Age: 40
Location: FL
Admitted: 07/21/2021
To: Baptist South
Murdered: 08/04/2021
Austin Miles
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.