
Steve Tomasi – Murder by COVID Protocols
Age: 62
Location: NM
Became sick: 11/01/2021
First sought care: 11/02/2021
Admitted: 11/08/2021
To: Lovelace Hospital
Murdered: 11/18/2021
Steven Anthony Tomasi



My Dad, Gary Wiegand, was an Army Veteran, a loving husband of 52 years, a father, beloved Pappap to 5 grandkids, father-in-law, brother, uncle and a friend to many. He was a gentle giant and one of the best guys in the universe.
My Dad was killed on 21 January 2022, when his “trusted” doctors following a hospital cv-protocol denied his rights to try safe & effective treatments, that are being suppressed. My family advocated for medications that greatly improved symptoms for my husband, friends, and acquaintances, within a 24-hour period. These low-cost, FDA-approved medications are doctor prescribed in other states, and countries, and have been used safely for decades. During the 12 days Dad was in UPMC Passavant, he was isolated, denied antibiotics, ventilated against his will, and heavily sedated. My Dad lived in Pennsylvania, a “Right to Try” state but for him it was a “Rights Denied” state.
On Monday morning, 10 January, Dad visited the UPMC Passavant ER. His symptoms started New Years Day. He had a negative home Covid test earlier in the week but this morning he was unsteady on his feet and needed to seek medical care. In the ER, he was tested for Covid, flu and pneumonia, administered iv-fluids, and given a breathing treatment. Upon learning he was not vaccinated, the ER doctor informed my Dad, “This is what happens when you don’t get vaccinated.” Dad’s vaccine status was irrelevant at that time considering medical professionals recommend against vaccinating someone who is ill. When Mom shared that Dad had a negative home test, the same doctor informed them, “the home tests are garbage.” After being told he was cv-positive, they admitted him to “monitor his breathing.” Dad’s pulmonologist, of 5 years, was a member of his care team. They were told Dad had an infection and they would treat it. They felt confident that Dad was in good hands and would be home in a day or two.
The next day, a non-emergent move to the ICU was made to “monitor his oxygen levels more closely.” Aside from having visitors for an hour a day, Dad was isolated, hearing & vision impaired, placed on a clear-liquid diet, and left without an advocate to ensure he could make informed decisions. When mom visited him he asked to go home. In reviewing Dad’s records, his pneumonia was left untreated and he was monitored off of antibiotics. His ER radiology report noted concern for pneumonia. In the reports from the following days, they noted his pneumonia is getting progressively worse. Our family was told Dad’s infection was being treated but he received no antibiotics until 18 January, after 9 days under their care.
On the morning of 13 January, Mom was informed that Dad was ventilated. During the early morning hours, he was agitated with the mask, complaining about the heated high flow, tried removing the bi-pap, and they needed to “rest his lungs.” In Dad’s records, a nurse noted that the “patient unaware of the risks to be intubated.” In talking with Dad’s nurse I learn that Dad is receiving all of his regular meds as well as dexamethasone, and continuous infusions of fentanyl, Propofol, sedatives, muscle relaxants, and paralytics. I ask about Ivermectin for Dad and am told “there are no FDA approved cv treatments.” I share my husband’s cv-pneumonia recovery story. In the end of July/early August 2021, my family had covid. Our youngest had no symptoms, my older kids and I were sick 3-5 days, my husband was the first one with symptoms and on day 10 ended up in the Alabama ER. My husband was sent home with Ivermectin, Azithromycin, Dexamethasone, a cough expectorant, and Zofran, all doctor-prescribed. His symptoms were improved within a 24-hour period and he felt relief within 3 hours of taking his first dose. Dad’s nurse will pass this information on to his doctors.
On Friday, 14 January, I met members of Dad’s care team and received a copy of the hospital cv-protocol. I am disappointed to see they will not prescribe high-dose IV vitamins, ivermectin, hydroxychloroquine, NAC, and other low-cost medications that have been effective. Dad’s doctor is on the defensive when he joins us in the waiting area and informs us that “I cannot and will not prescribe Ivermectin for your Dad.” Mom asks me to share my husband’s cv-recovery story and I press him for a medical reason why he can’t prescribe this medication. He doesn’t give us one. Instead, we were told “It’s not the hospital cv-protocol”, they “would lose their license if they prescribe anything not on the protocol”, and they “won’t prescribe anything that could be potentially harmful to a patient.” Is there a prescription drug that could be more harmful than death? How is an inexpensive drug that has been used safely for decades, is a 2x Nobel prize winner, and is on the NIH essential medicine list now harmful to cv patients? They’re not even prescribing vitamins and according to Dad’s doctor, “vitamins don’t work.” My functional medicine doctor would disagree and we advocate for vitamins C, D and zinc.
We inquired about Hydroxychloroquine, an inexpensive drug that has been used by the military and repurposed for patients to treat chronic illnesses, for decades. Dad’s doctor informed me that “with every question you ask me and the nurses, you are taking care away from your Dad and the other ICU patients”, and told us to “forget about all the information you researched and spend time with your Dad.” We’re told that, surprisingly, “Gary is handling the vent well because we usually see a steady decline within the first 12 hours.” He also shared that he believes Dad “has a 25% chance of walking out of the hospital.” If his chances of leaving are so low why are they not trying everything possible to save his life? He tells us “if you want Gary to have any medications not on the protocol we should “file for a court order and hire a nurse to administer the drugs.” He also encourages us to “think about what Gary would want” and he tells us that “as an ICU doctor I would never choose to be vented.” Doctors have prescribed FDA-approved medications, off label, for decades and they are refusing to prescribe the medications that worked for my husband. We are concerned our advocacy efforts could impact Dad’s quality of care but over the next 7 days, we push for effective treatments but it feels as if they are just waiting for him to die. On day 8, we’re told that Dad’s cv-pneumonia has cleared and he’s dealing with inflammation. We asked his doctor about using Ivermectin again and he informed us, “I already put my neck on the line to prescribe vitamins.” Dad’s inalienable rights to try FDA-approved medications continue to be denied and we’re told “it’s not the hospital cv-protocol.”
On 20 January, Dad’s doctor informs us that he has 3 hospital-acquired infections, one of which is sepsis. My mom asks about dialysis for Dad but “he doesn’t qualify because his kidneys are functioning.” We’re told we “need to consider comfort care and think about what Gary would want.” His doctor encouraged us to take Dad off the vent and let him go. The rules no longer apply and we have unlimited time with Dad.
On 21 January, comfort measures and flipping from prone to supine are the goals on Dad’s white board. His doctor asks for a DNR. He explains that Dad’s infections have caused damage beyond repair and performing CPR would only cause more. At 8:28pm, my Dad’s heart stopped. Shortly after, his doctor comes in the room and he doesn’t talk to or even look at me! Is it possible that he knows he didn’t do everything he should have because of the hospital cv-protocol? Was Dad treated differently because he didn’t have the vaccine? If Dad’s pneumonia was treated on the day he was admitted would he have been discharged within a few days, would he have required ventilation, and would he even be dead?
The day after Dad’s death, his medical record portal is no longer accessible. In the days that follow, we also receive a letter from UPMC Passavant expressing their condolences, informing us of Dad’s lower respiratory tract infection, and “In a commitment to transparency” they offer to answer our questions. We learn that the letter is the “Infection Letter” required by Pennsylvania Law. It’s to notify us of the hospital acquired infections that Dad had but it makes no mention of these infections. I express our concerns and ask more questions. The representative needs time to gather some information and will follow up with me in a few days. I don’t hear from her and when I follow up, she informs me that “I was advised not to call you back or answer your questions because they were already answered.” I request contact information for the person who told her that. When I contact the supervisor, I’m told another letter was sent to my Mom, my questions have been addressed, and there’s nothing else they can do for us. I express concerns over their cv-protocol, the “commitment to transparency” while also having a “lack of transparency” with their “Infection letter,” I share my husband’s Ivermectin recovery and conversations that were had with Dad’s doctors. I’m told they won’t prescribe anything potentially harmful to patients, those conversations didn’t happen, and she apologizes that his doctors didn’t explain things better. Dad’s doctors were very clear and I know that their cv-protocol suppressed low-cost, safe and effective, FDA-approved, doctor-prescribed medications that my husband and others received, they placed profit over patient lives, and my Dad’s blood is on their hands.
Filter By Category

Age: 62
Location: NM
Became sick: 11/01/2021
First sought care: 11/02/2021
Admitted: 11/08/2021
To: Lovelace Hospital
Murdered: 11/18/2021
Steven Anthony Tomasi

Age: 54
Location: PA
Became sick: 11/09/2021
First sought care: 11/09/2021
Admitted: 11/14/2021
To: Evangelical Community Hospital Lewisburg Pa
Murdered: 11/18/2021
Matthew Smith

Age: 40
Location: FL
Became sick: 07/16/2021
First sought care: 07/21/2021
Admitted: 07/21/2021
To: Baptist South
Murdered: 08/04/2021
Austin Miles
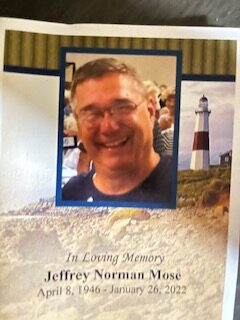
Age: 76
Location: MI
Became sick: 01/03/2022
First sought care: 01/04/2022
Admitted: 01/08/2022
To: Beaumont Hospital, Troy, MI
Murdered: 01/26/2022
Jeffrey Norman Mose

Age: 56
Location: ID
Became sick: 08/22/2020
First sought care: 08/24/2020
Admitted: 08/26/2020
To: St Alphonsus Med Ctr
Nurse Patti Gilliano

Location: PA
Became sick: 08/26/2021
First sought care: 08/28/2021
Admitted: 09/01/2021
To: St Lukes Fountain Hill Bethlehem, Pa
Murdered: 09/13/2021
Christopher F. Loncaric

Age: 79
Location: VA
Became sick: 04/15/2021
First sought care: 04/30/2021
Admitted: 04/30/2021
To: St Francis Medical Center
Murdered: 05/30/2021
Carol K Vaughan

Age: 69
Location: NV
Became sick: 08/22/2021
First sought care: 09/01/2021
Admitted: 09/01/2021
To: Southern Hills Hospital
Murdered: 09/26/2021
Steven R. Blatt
Age: 59
Location: PA
Became sick: 04/09/2021
First sought care: 04/16/2021
Admitted: 04/18/2021
To: Delaware County Community Hospital
Murdered: 04/30/2021
Michael Shalon SR

Age: 51
Location: SC
Became sick: 08/30/2021
First sought care: 09/03/2021
Admitted: 09/06/2021
To: MUSC, Scouth Carolina
Murdered: 09/21/2021
Ian Bonnet

Age: 59
Location: AZ
Became sick: 11/01/2021
First sought care: 11/08/2021
Admitted: 11/08/2021
To: Banner Del E. Webb medical center
Murdered: 12/07/2021
Miguel Rodriguez

Location: MO
Became sick: 08/03/2021
First sought care: 08/15/2021
Admitted: 08/15/2021
To: Cox North
Murdered: 08/23/2021
James and Shirley Flowers

Age: 49
Location: OR
Became sick: 12/26/2021
First sought care: 01/02/2022
Admitted: 01/02/2022
To: 1/2/22 Legacy Meridian transferred 1/5/22 to OHSU
Murdered: 02/24/2022
Patrick Perales

Age: 61
Location: OH
Became sick: 09/13/2021
First sought care: 09/13/2021
Admitted: 09/13/2021
To: Genesis hospital
Murdered: 10/02/2021
William Darrell Lyons

Age: 55
Location: GA
Became sick: 12/09/2020
First sought care: 12/10/2020
Admitted: 12/17/2020
To: Northside Gwinnett
Murdered: 01/20/2021
Tony Dana

Age: 71
Location: MI
Became sick: 11/24/2021
First sought care: 11/24/2021
Admitted: 11/24/2021
To: McLaren Hospital, Mount Clemens
Murdered: 01/02/2022
Charles V. Domine; aka Chuck
Age: 83
Location: FL
Became sick: 08/17/2021
First sought care: 08/20/2021
Admitted: 08/22/2021
To: Florida Hospital Altamonte Springs
Murdered: 08/29/2021
Mark P. Kingsley

Age: 64
Location: TX
Became sick: 09/01/2021
First sought care: 09/06/2021
Admitted: 09/11/2021
To: John Peter Smith Hospital and THR Arlington Memorial
Murdered: 09/27/2021
Michael Weedman
Age: 54
Location: CA
Became sick: 08/01/2021
First sought care: 08/13/2021
Admitted: 08/13/2021
To: Kaiser Permanente, Santa Clara, CA
Lena Spasioti

Age: 47
Location: VA
Became sick: 03/02/2021
First sought care: 03/02/2021
Admitted: 03/02/2021
To: VCU Richmond
Murdered: 08/29/2021
Sarah Dick

Age: 57
Location: OH
Became sick: 12/11/2021
First sought care: 12/17/2021
Admitted: 12/17/2021
To: Aultman
Murdered: 12/27/2021
Kenneth Mehalic

Age: 74
Location: NJ
Became sick: 12/20/2021
First sought care: 12/20/2021
Admitted: 12/27/2021
To: Virtua, Lady of Lourdes, Camden
Inez Delfico and Otto "Butch" Moring

Age: 28
Location: IN
Became sick: 01/20/2021
Murdered: 01/21/2021
Haley Link Brinkmeyer

Age: 59
Location: OK
Became sick: 08/06/2021
First sought care: 08/10/2021
Admitted: 08/11/2021
To: Saint Francis Hospital South
Murdered: 08/31/2021
Laurie Dwyer
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.