
My husband mattered!!
Age: 60
Location: MI
Admitted: 04/03/2021
To: McLaren Northern Michigan Hospital
Murdered: 05/05/2021
Paul Kucharek


In February of 2021, I was at an appointment with my endocrinologist when she asked me if I planned to get the COVID vaccine when it became available to us. I simply told her, “No”, fully expecting a lecture. She asked me if it was because of the potential side effects and I simply answered, “Yes.” She then looked up at me and nodded as though she understood and told me that I was very healthy and unlikely to get very ill if I did catch the virus.
On Monday, July 26, 2021, I went to work in the laboratory of the hospital where I would later become a patient, but left after a couple hours when I felt the slightest of coughs and body aches come on. I went to the Urgent Care down the road to get swabbed for the PCR test and seen by a PA. The PA called me the next day with the positive test result.
Over the next 5 days, I would quickly develop all of the mild to moderate symptoms and was essentially bedridden. Living alone, I did my best to try to take care of myself, but when I became dehydrated and my cough became incessant, I drove myself to the ER of the hospital where I work.
There, I was given IV fluids and stronger cough meds then discharged to home after being told I wasn’t sick enough to admit. At no point during these first 5 days of illness did any provider even mention to me that I met the CDC criteria for monoclonal antibody treatment that could help prevent serious illness and hospitalization.
The next day, Sunday, August 1, I felt significantly better and assumed I had seen the worst of what the virus would do to me. The following 2 days saw my breathing become more difficult and on August 3, I had to call an ambulance to take me back to the ER with a blood oxygen saturation of only 67%.
Working in the hospital lab, I knew that the outcome for COVID patients in the ICU was, to my knowledge, always death, but I did not understand at that point that the treatment protocols were essentially a death sentence. I was terrified to go to the hospital because I knew that I was going to end up on a ventilator with how I was now in respiratory distress, but my ability to treat my condition at home was no longer an option once the cytokine storm hit me.
I was admitted as an ICU patient to the back up ICU unit. The next day, August 4, I was moved into the real ICU and prepped with an arterial line and PICC line then intubated and placed on the ventilator. I was supposed to be on the vent for 3 full days, but on August 6, despite being sedated and in wrist restraints, I unknowingly wiggled down in my bed, grabbed onto the endotracheal tube and pulled it out. I have a vague memory of sitting up quickly in my bed gasping to try to breathe while several people ran into my room in a panic. I was then placed on a bipap mask with forced oxygen therapy for the next 4 days to try to keep my O2 saturation above 90%.
On August 9, they suspected that I had developed a pulmonary embolism and took me for a CT scan which confirmed just that. I was then placed on a heparin drip for the rest of my stay in the ICU. On August 10, my 55th birthday, I was struggling to keep my O2 sat high enough, even though I was maxed out on 100% oxygen at 8 L/m on the bipap. The nurse informed me that I was going to have to go back in the ventilator to help me breathe. As she was making preparations and awaiting the anesthesiologist and nurse anesthetist to arrive, I was able to text my oldest sister who was my Health Care Power of Attorney to make her aware so she could be sure to keep in touch with the nurses and doctors.
This was the only one of the 3 times I was placed on the ventilator that I remember the moments leading right up to being intubated. I was reflecting on how back in July of 2000, my 5 older siblings and I gathered around our mother’s ICU bed as they took her off the ventilator, and we watched as her body struggled to take its last few breaths. I was worried that my siblings would have to make that decision for me without being able to be there to see me one last time. I still have little post traumatic stress as I recount these parts of my story. With my head cocked back as the anesthesiologist positioned to intubate me, I wondered if that was going to be my last moment of consciousness in this life as I watched the nurse anesthetist inject the sedation meds into my IV line.
Looking back at a text message, I messaged someone on August 23 that I was now awake and alert again. Thinking I had been on the vent for the last 13 days, I had to learn from my sister that I had actually been on the vent for only 3 days, but I was kept intubated, sedated but breathing on my own power for an additional 10 days with the oxygen going through the endotracheal tube, rather than waking me up and placing me back on the bipap mask. I also learned that during my second day on the vent that time, August 11, that there was a Cardiac Arrest Code called overhead for me. I was told when my coworkers in the lab heard this announcement, they all stopped and stared in silence at each other.
My sister was called by a nurse to inform her that I had gone into cardiac arrest, and that they would call her back right away as soon as they knew more. My sister waited 2 hours before she called the ICU to ask what had happened to me. It turned out that I didn’t go into cardiac arrest. Because I had pulled out my endotracheal tube the first time I was on the vent, they decided to increase my sedation meds this time. The high dosage of sedation meds made my heart rate slow so much that a nurse thought that I was in cardiac arrest.
When the doctor showed up to the room for the code, he quickly realized what had happened. A couple phlebotomists who I work with in the lab told me that I had had a few cardiac arrests called on me, because they are the ones who respond to them from the lab. I still have to comb through my medical records to see if there is documentation of these incidents there. These coworkers also told me that one particular nurse always seemed to be the one who was asssigned to me every time my condition seemed to take a turn for the worse. They half-jokingly tell me that she was trying to kill me. That nurse no longer works there to my knowledge.
I at first thought that I was then on the bipap mask for 1 week before being placed back on the vent on August 30, but when reviewing my medical records I saw a report from a chest x-ray from August 24 that commented on the placement of my endotracheal tube. When my sister checked her notes, she conferred that I was intubated and placed back on the vent for the third time on August 24. That means I was only awake and alert for maybe 1 day from the 23rd to the 24th.
I do remember an extremely emotional Zoom meeting that I had with 3 of my siblings to discuss the decision I had to make regarding a recommendation from the physicians, so that must have taken place on August 23rd. I was told that I would have to be placed back on the vent for a length of time that they could not predict, and that they they would not want to keep me intubated the entire time. That would require that I have a tracheostomy tube surgically placed at some point, and have the vent switched from the endotracheal tube to the trach tube. This carried several risks that required my consent. I determined that if I got to that point, that my odds of survival were very low, but I wanted to take that risk and therefore it would be in the hands of my siblings to decide when to end my life.
So after being placed on the ventilator the 3rd time on August 24th through an endotracheal tube, I then had the tracheostomy tube inserted on August 30 and the vent switched over to that entry.
Per system wide hospital protocols, I was not allowed any visitors for the first 28 days in the hospital, but my sister was not able to visit the first time until September 2nd. When she did, I was still on the vent, burning up with a fever that the day nurse was doing nothing to address. When the night nurse came in, she packed me in ice to bring the fever down. The next day when my sister visited, I was pale, cold and completely unresponsive. It was then when she and my other siblings had to begin the discussion of how much longer to keep me alive on the vent.
I must have begun to show some signs of responding over the next day as my sister and her husband visited. I don’t understand how this worked, since I have no conscious memory of it, but I must have been able to interact somewhat while sedated. My brother-in-law had asked if I wanted him to anoint me with oil and pray over me, and I’m told I responded in the affirmative. Dozens of people, most of whom I’ve never met, were praying for me during this time.
The day after he prayed over me, I began to show signs of improvement. So much so that from September 5 into September 8, they weaned me off the ventilator. I was allowed to breath on my own power while awake, but switched back over to the ventilator at times, especially while sleeping. By September 8th, I was completely off the ventilator. I was moved out of the ICU in the middle of the night on September 9/10 into a regular room on a Med/Surgical unit. I was then transferred to the Inpatient Rehab unit and on September 24, 52 days after being admitted, discharged from the hospital.
On September 10, my pulmonologist visited me and told me that I had a “remarkable and miraculous recovery,” due to the fact that essentially everyone who had gotten as ill as I was had died.
There was a moment while I was heavily sedated, I believe it was September 4, when I had an unusual clarity of mind. During this time, I came to realize how long I had been in the ICU and how long I had been on the vent and that I was getting worse, not better. Not knowing that everyone believed that I was almost certainly going to die, I came to that realization myself. In fact, I had gotten to my breaking point where I told God that he needed to end this somehow very soon, because I couldn’t take the suffering any longer. I needed it to end very soon and was making peace with the fact that I would die soon. But then I became overwhelmed with deep sadness.
I had always sought to try to give of myself sacrificially to others as a help and encouragement, only to always be misunderstood, falsely accused, betrayed and abandoned by those closest to me, much like Jesus had and has. I had always viewed my various adversities and sufferings in life as opportunities to learn, grow and develop my character to someday be used by God to help others. When I realized that all that I had seen as preparation was now going to be wasted with my life coming to an end, I was saddened and feeling like a failure. But it wasn’t the end. God worked a miracle to save me from the deadly protocols.
I have been divorced twice, and have no children of my own. No one would have had their life changed drastically if I had died. When I began hearing stories of those who had died and left behind spouses and young children, I would wish that God had given me the choice to accept His miracle or give it away to someone who had people who depended on them. I would have chosen to give it away.
After I returned to work in the lab of the hospital where I was nearly killed, we had a 48 year old man with COVID in our ICU on the ventilator. One of my lab coworkers knew this man’s family. While I was working with her one Sunday, unknown to me she had received word that this man’s wife had made the excruciating decision to take him off the vent and let him go, leaving her to raise their children without him. My distraught coworker came up to me and said, “There better be a good reason why you lived. God better have something important for you to do!” I can only hope that God uses the story he has given me to tell to be a voice for those who have had their lives and own voices taken from them. Whatever I can do, I am willing to do it. I may still work for the employer that tried to kill me like it did so many others with their protocols, but I am not afraid of them. They had better be afraid of me and the story I have to tell.
Filter By Category

Age: 60
Location: MI
Admitted: 04/03/2021
To: McLaren Northern Michigan Hospital
Murdered: 05/05/2021
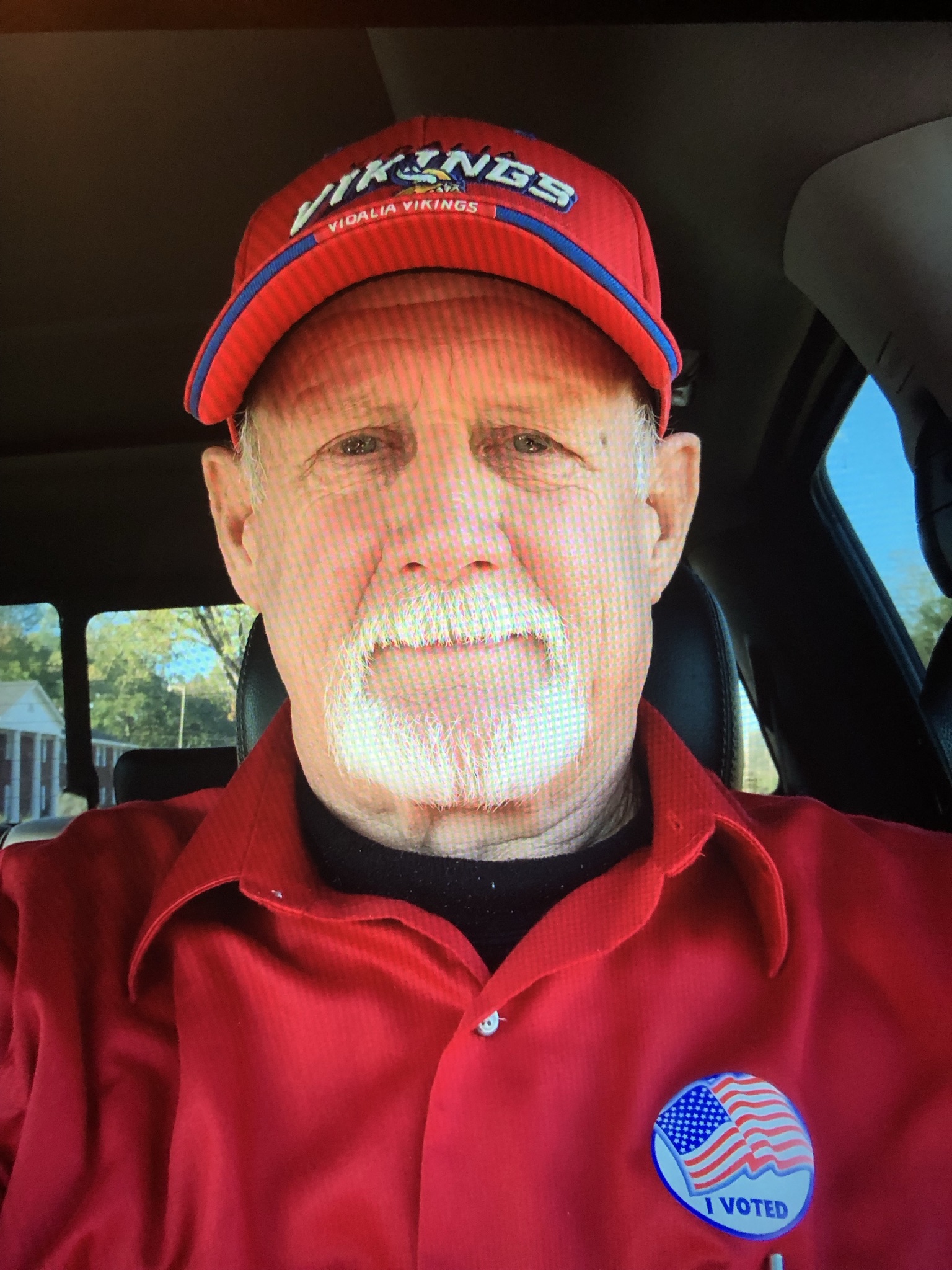
Paul Kucharek
Age: 77
Location: FL
Admitted: 07/09/2021
To: Jackson Hospital, Marianna FL
Floyd Hansbury

Age: 51
Location: CA
Admitted: 01/10/2021
To: Torrance Memorial
Murdered: 02/16/2021
Joseph Dale Christopher
Age: 68
Location: MS
Admitted: 08/03/2021
To: Merit Health Natchez, 8/3/21 and Merit Health Vicksburg Rehabilitation floor 9/28/21
Murdered: 10/19/2021
Forrest D Foster
Age: 70
Location: CA
Admitted: 10/11/2021
To: Bakersfield Heart Hospital
Murdered: 10/26/2021
James Jackson, III (Sonny)

Age: 66
Location: FL
Admitted: 07/15/2021
To: Palms West Hospital in Loxahatchee, Florida (Palm Beach County)
Murdered: 08/01/2021
Michael H. McVan

Age: 78
Location: IL
Admitted: 11/19/2021
To: Delnor Hospital, Elgin, IL
Murdered: 11/30/2021
Sherri Ronstadt

Age: 70
Location: PA
Admitted: 12/25/2021
To: Penn State Holy Spirit Hospital
Murdered: 01/15/2022
Clair W. Hoffman

Age: 51
Location: MI
Admitted: 10/17/2021
To: Mclaren Lansing
Murdered: 10/28/2021
Geoffrey e Bruce

Age: 32
Location: WA
Admitted: 09/23/2021
To: St Joseph PeaceHealth
Murdered: 10/14/2021
Phillip Carron

Age: 73
Location: IL
Admitted: 12/30/2021
To: Advocate Sherman Hospital
Murdered: 01/27/2022
Tom Coronado 2

Age: 59
Location: AZ
Admitted: 01/05/2022
To: Baywood Hospital
Murdered: 01/20/2022
Tammy Bay

Age: 34
Location: OR
Admitted: 08/12/2021
To: Bay Area and transferred to McKenzie Willamette
Murdered: 08/26/2021
John F. Waller "Johnny"

Age: 68
Location: CA
Admitted: 07/23/2021
To: Sharp Memorial Hospital
Murdered: 08/08/2021
David Charles Coleman

Age: 19
Location: WI
Admitted: 10/07/2021
To: Ascension St Elizabeth in Appleton
Murdered: 10/13/2021
Grace Schara

Age: 65
Location: TX
Admitted: 11/27/2020
To: Shannon Medical Center
Murdered: 01/14/2021
Danny Ray Simmons

Age: 76
Location: IN
Admitted: 01/13/2022
To: Riverview in Noblesville, Indiana
William Lyman

Age: 87
Location: FL
Admitted: 03/22/2019
To: University Hospital Tamarac Florida
Murdered: 05/25/2019
Vincent Gentile

Age: 59
Location: NY
Admitted: 10/02/2021
To: Saint Catherines
Stanley j. Czarnecki

Age: 55
Location: NV
Admitted: 08/30/2021
To: Centennial Hills Hospital
Murdered: 09/23/2021
Ricardo Fimbres

Age: 54
Location: FL
Admitted: 07/31/2021
To: Orlando Regional Medical Center
Murdered: 07/14/2022
Dexter G Sullivan Jr

Age: 52
Location: KS
Admitted: 01/27/2022
To: Overland Park Regional
Murdered: 02/07/2022
Marc Saulnier

Age: 51
Location: SC
Admitted: 08/17/2021
To: Trident Medical Center
Murdered: 09/01/2021
Byron Kendziora

Age: 74
Location: AZ
Admitted: 10/30/2021
To: Banner Thunderbird Medical Center
Murdered: 12/14/2021
Linda Mary Wilson
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.