
The absolute negligence, and belligerence in killing my wife with Decadron and Remdesivir!!!
Age: 82
Location: AK
Admitted: 11/28/2020
To: Mat-Su Regional Medical Center
Murdered: 12/09/2020
Mary Louise ( James) Nelsen


Friday, April 8,2021 Steve had a sore throat. On Saturday he went to Rocket testing and was confirmed positive for Covid 19. I was negative. At this point he was feeling well, just a scratchy throat. On Monday, we both went to Walgreens for a test and both tested positive. On Tuesday we both had fevers. Mine subsided, but Steve ran a very high fever for days. On Friday, his breaths per minute was elevated. I called the hospital and they said they would have someone call me. I waited till midnight with no call.
In the morning I called again said to bring him to the Satellite care center who told us to go right to the Lake Forest hospital emergency room. In their “review of systems”, said positive for appetite change, chills, diaphoresis, fatigue, and fever. Negative for sore throat, negative for chest tightness and shortness of breath, negative for chest pain and leg swelling, negative for abdominal pain, diarrhea, and vomiting, positive for decreased urine flow, and positive for weakness. BP 138/74, pulse 75, temp 99.9, resp 28, and sp02 91%. Physical exam: General: He is not in acute distress. Appearance : He is not toxic appearing. Eyes: no scleral icterus. Cardiovascular: Normal rate and regular rhythm, normal heart sounds. Pulmonary: normal breath sounds, MILDLY TACHYPNEIC. (They highlighted on the report). Skin warm and dry. Neurological: He is alert.
With a report like this you can see he wasn’t that sick. They admitted him, gave him oxygen. I talked to him and he was alert and resting. On 4-17, day of admission they gave him Remdesivier. Why???? After that everything went downhill. His Ddimer numbers went from 500 to 69,000 as high as the lab could go. All his stats plunged. On 4-20, they intubated him telling me if they didn’t, he was going to die. The Dr. even warned me the day before he wanted to and I told him I didn’t want him on a ventilator.
After 4 days on Remdisivier, his kidneys failed and needed dialysis, blood clots in his arms, “covid” pneumonia, liver failure, and more. After 11 days they tried to take him off the ventilator and was off 5 days and had to put it back in. This happened again and vented again for the 3rd time with a trache. During this time he was pumped with fentynol, morphine and many other drugs . He laid there unconscious and alone for 51 days, lost 50 pounds, had bed sores the size of a volleyball, wounds on his face, all his skin peeling from his body because of endemia, and everything else that is done to someone in a coma.
On May 28th, his lung collapsed and they were able to revive him. They put tubes in his lungs to drain the fluid from the damage the ventilator does to the lining of the lungs. God heard all our prayers and was surely with him as they realized he wasn’t going to die for them. They later transferred him to RML, a LTAC. (Long Term Acute Care hospital) who specializes with patients on ventilators and traches. On June 7th was the 1st day I could see him. When I saw him, I was in shock. He was a skeleton, unshaven, unbathed, tape marks all over his body etc. I spent 10 hours a day with him, everyday, shaving, cleaning him, cutting his hair etc. He was in the LTAC from 6-7 to 6-13 and went to Amita Hinsdale ICU for partial collapsed lung.
They admitted him and here they inserted a 3rd tube in his left lung. He returned to RML on 6-24-21. On 7-20-21, they were collapsing again so went back to the Hinsdale ICU. Here again, they called in a thoracic surgeon. Steve’s lungs were so bad they were talking lung transplants but too weak etc. Dr. Gordon put 2 more “garden hoses” tubes into his pecs. Once he was stable, they moved him back to RML on 7-27-21. RML’s job was to get him off the ventilator which they did by the time he left, but left the trache in for emergency use. During this time, he couldn’t even pick up his cellphone, sit up in bed or eat. Finally he was moved to Shirley Ryan Rehabilitation, downtown Chicago on 8-11. He couldn’t even sit in a chair at this point.
He was there till 9-8-21. I was told by many he would never fly again, would need a lung transplant, and be on oxygen for life. He went home with a wheelchair, oxygen, walker, and bath assist. He then spent the next 12 weeks doing outpatient therapy. During this time, we lost our business, and income as he can no longer work. This was the most horrifying time in our lives and I believe they tried to kill him with the remdisivier. I am thankful to God for saving my husband. Because of Steve’s determination and work ethic he is doing much better now after all his therapy.
Filter By Category

Age: 82
Location: AK
Admitted: 11/28/2020
To: Mat-Su Regional Medical Center
Murdered: 12/09/2020
Mary Louise ( James) Nelsen

Age: 68
Location: GA
Admitted: 08/21/2021
To: Gwinnett Medical
Murdered: 08/31/2021
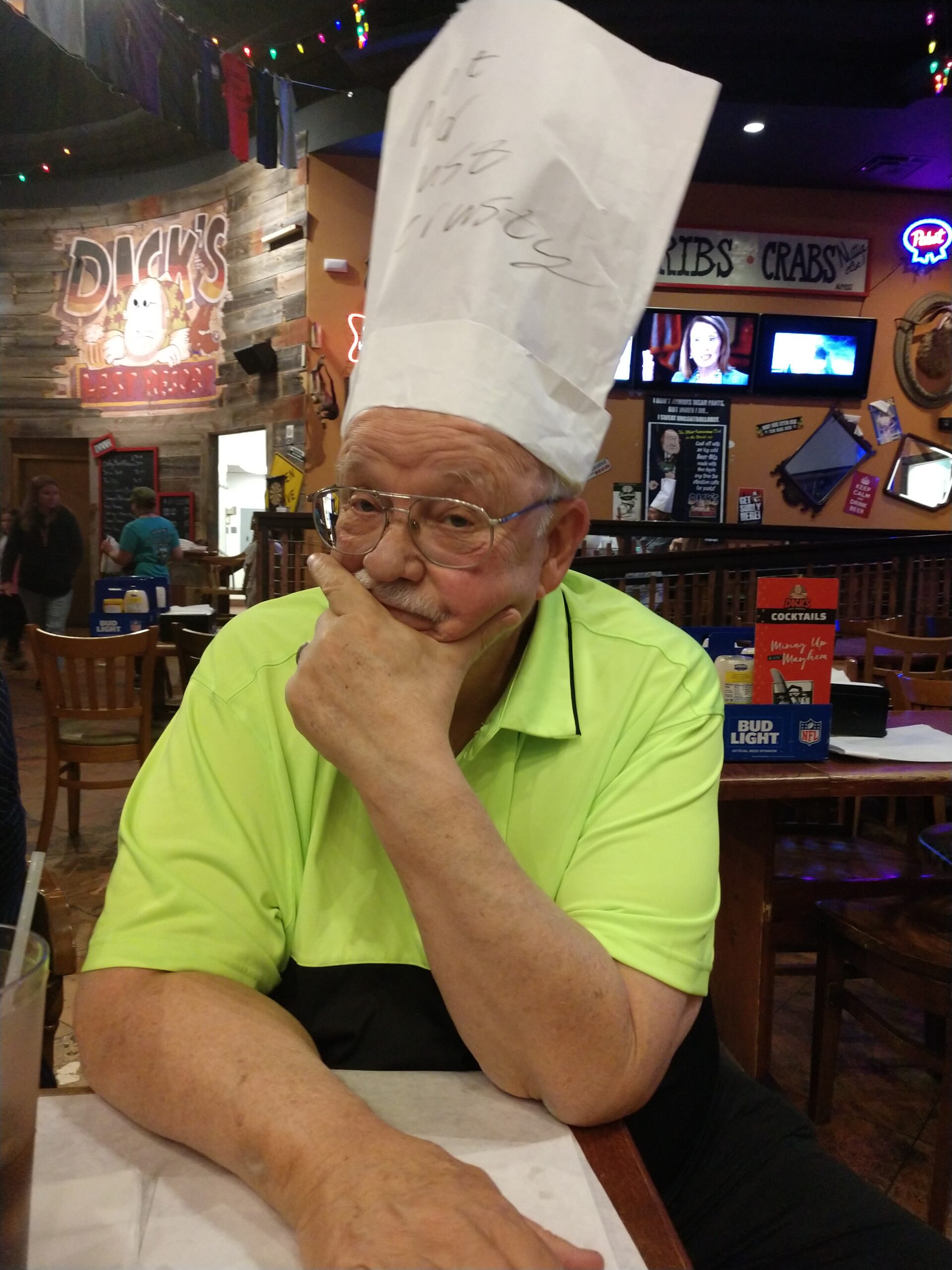
Steve Johnson

Age: 64
Location: OH
Admitted: 09/09/2021
To: Avita Hospital in Ontario Ohio
Murdered: 09/22/2021
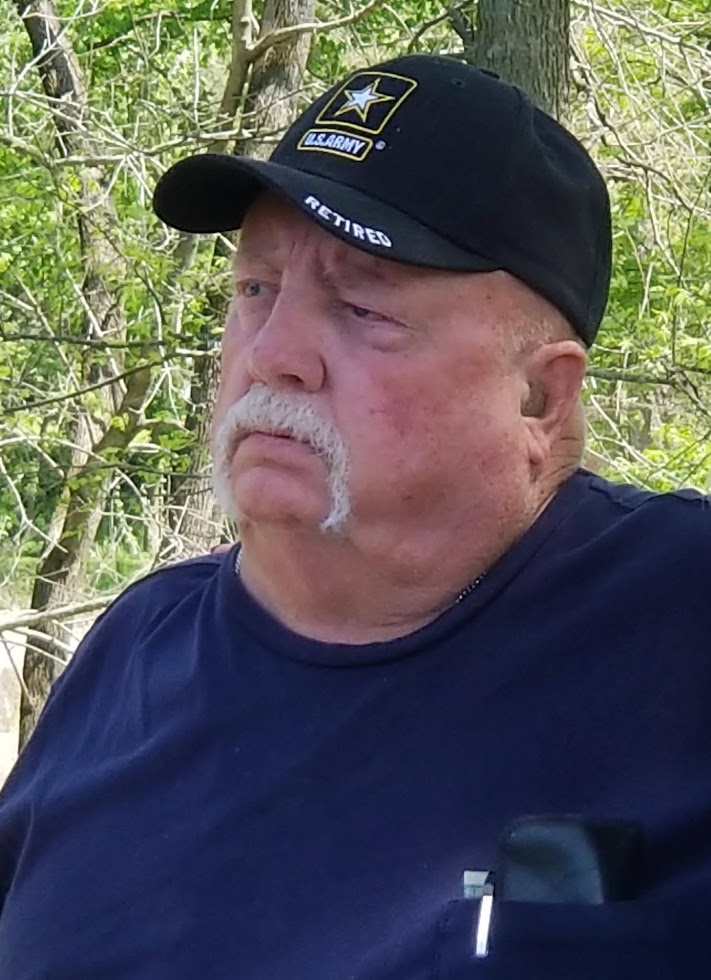
Ronnie Keith Brock

Age: 58
Location: NC
Margaret Love
Age: 72
Location: ND
Admitted: 05/07/2021
To: Sanford Medical Center Bismark, ND
Murdered: 05/17/2021
David Wolfer

Age: 67
Location: CO
Admitted: 11/11/2021
To: St. Anthony North Campus
Murdered: 11/26/2021
Steve Montoya

Age: 68
Location: CA
Admitted: 06/05/2020
To: Kaweah Delta Hospital
Murdered: 06/16/2020
Nellie Fernandez

Age: 58
Location: MD
Admitted: 01/15/2022
To: Ascension St. Agnes
Murdered: 01/21/2022
Anthony Battle

Age: 62
Location: CO
Admitted: 10/17/2022
To: Sam- Saint Anthony / Andrew - Lutheran Medical
Murdered: 11/05/2021
Samuel Miller and Andrew Miller

Age: 84
Location: PA
Admitted: 12/26/2020
To: Holy Redeemer Hospital
Murdered: 01/11/2021
Margaret(Peg) Rybas
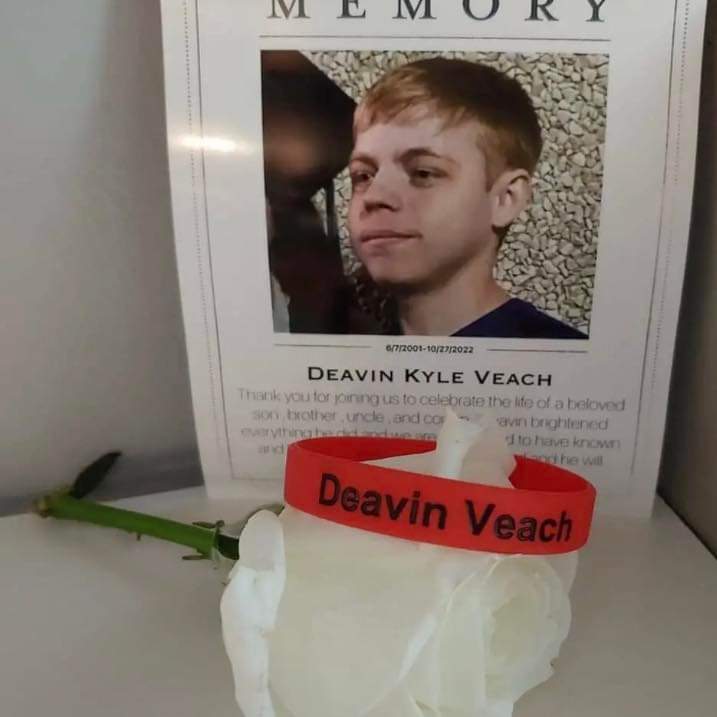
Age: 21
Location: OH
Admitted: 01/23/2022
To: Anderson Mercy Cincinnati Ohio,UC hospital Cincinnati Ohio, Christ hospital Cincinnati Ohio, Bethesda North hospital Montgomery Cincinnati Ohio
Murdered: 10/27/2022
Deavin Veach

Age: 52
Location: FL
Admitted: 03/14/2021
To: Jess Parrish
Murdered: 04/21/2021
Joe (Jose) Bowman

Age: 64
Location: NY
Admitted: 10/01/2022
To: Admitted after 36 hrs in ER
Constance Collins

Age: 62
Location: MI
Admitted: 04/26/2021
To: Henry Ford Hospital
Murdered: 05/04/2021
Francesco Todaro

Age: 43
Location: TX
Admitted: 08/07/2021
Murdered: 08/23/2021
Earl C Butler IV

Age: 60
Location: MI
Admitted: 11/17/2021
To: Sparrow Hospital Ionia Michigan
Murdered: 12/13/2021
Jeffrey Jay Marshall
Age: 83
Location: IA
Admitted: 05/03/2021
To: Greater Regional Medical Center and Des Moines Lutheran Hospital
Murdered: 05/21/2021
Charlene Pierce

Age: 48
Location: IA
Admitted: 12/28/2021
To: Mercy Westlake
Murdered: 02/28/2022
Darryl Van Holton

Age: 28
Location: IN
Murdered: 01/21/2021
Haley Link Brinkmeyer
Age: 72
Location: AR
Admitted: 11/26/2020
To: Yes
Murdered: 12/17/2020
Douglas A. Morriss

Age: 76
Location: FL
Admitted: 01/14/2022
To: Woodmont HCA
Murdered: 02/01/2022
Ina Kunis

Age: 55
Location: FL
Admitted: 08/29/2021
To: Parish Medical Center
Murdered: 10/11/2021
Dianne Spangler

Age: 51
Location: CA
Admitted: 01/10/2021
To: Torrance Memorial
Murdered: 02/16/2021
Joseph Dale Christopher

Age: 64
Location: UT
Admitted: 10/22/2021
To: St Johns
Murdered: 01/07/2022
Father Ubald Rugirangoga
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.