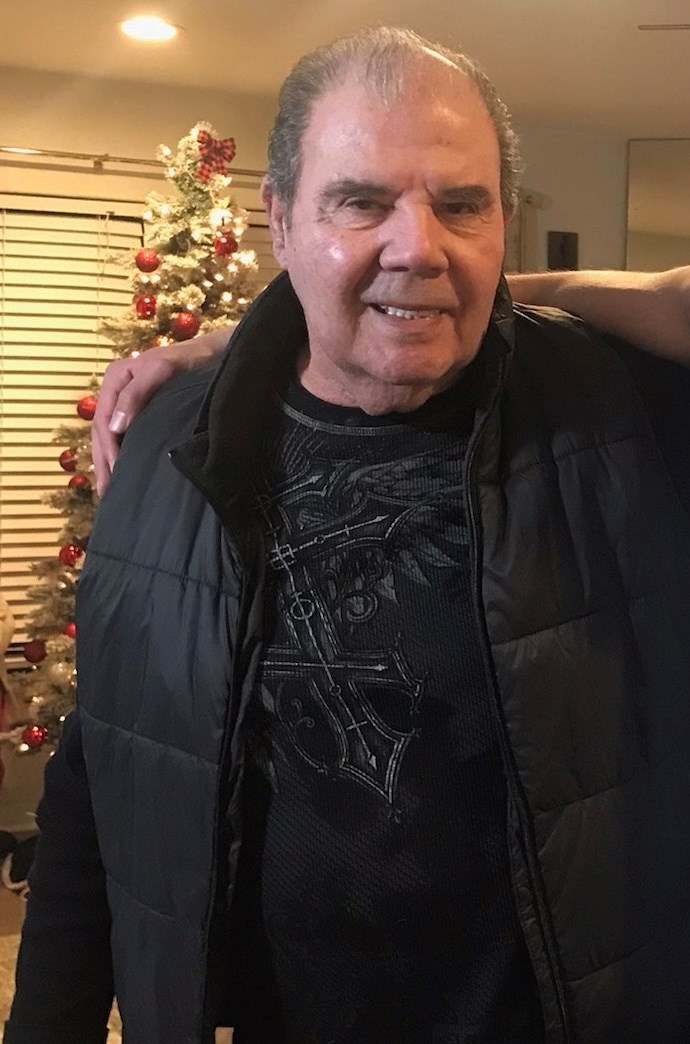
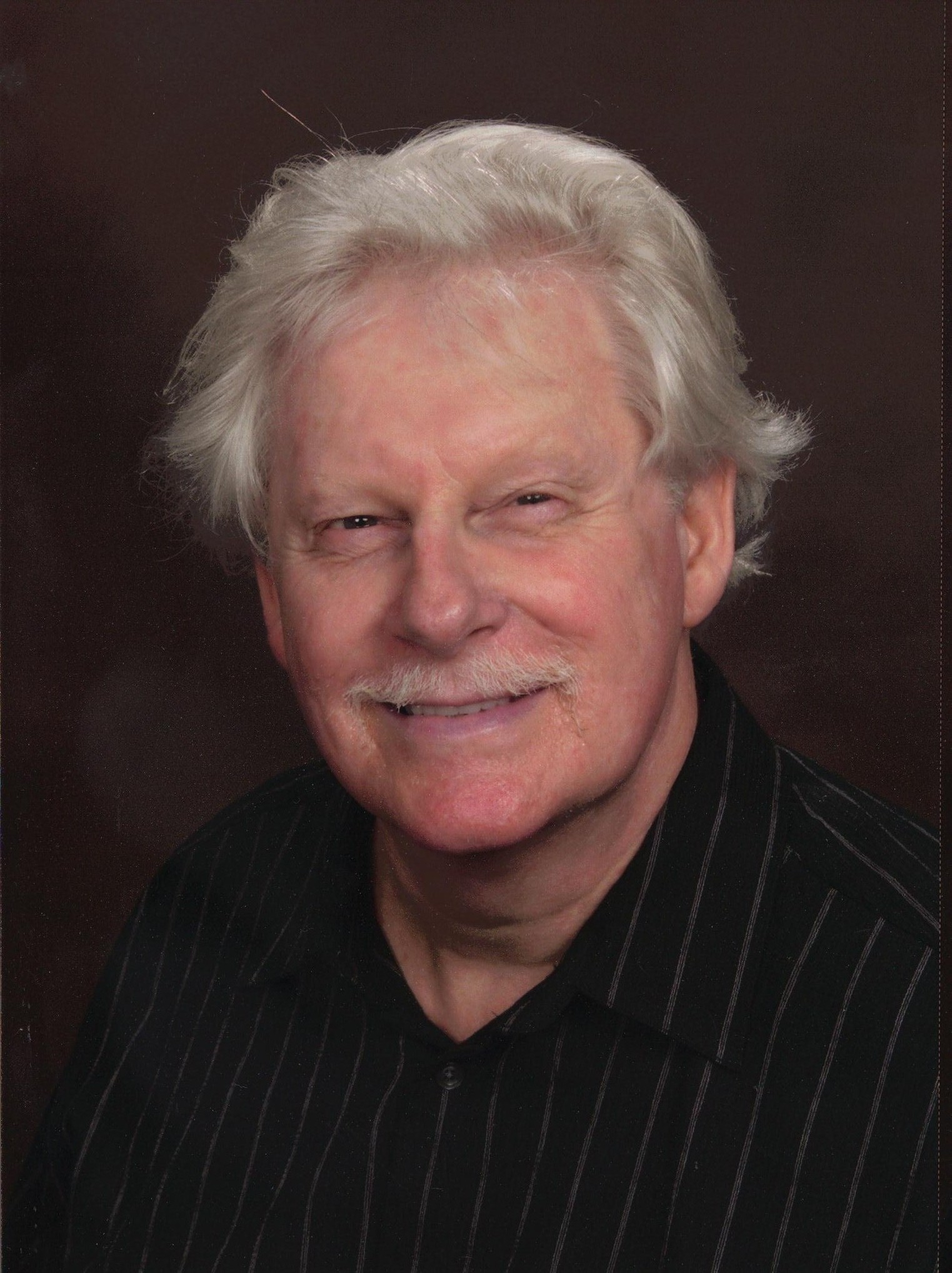
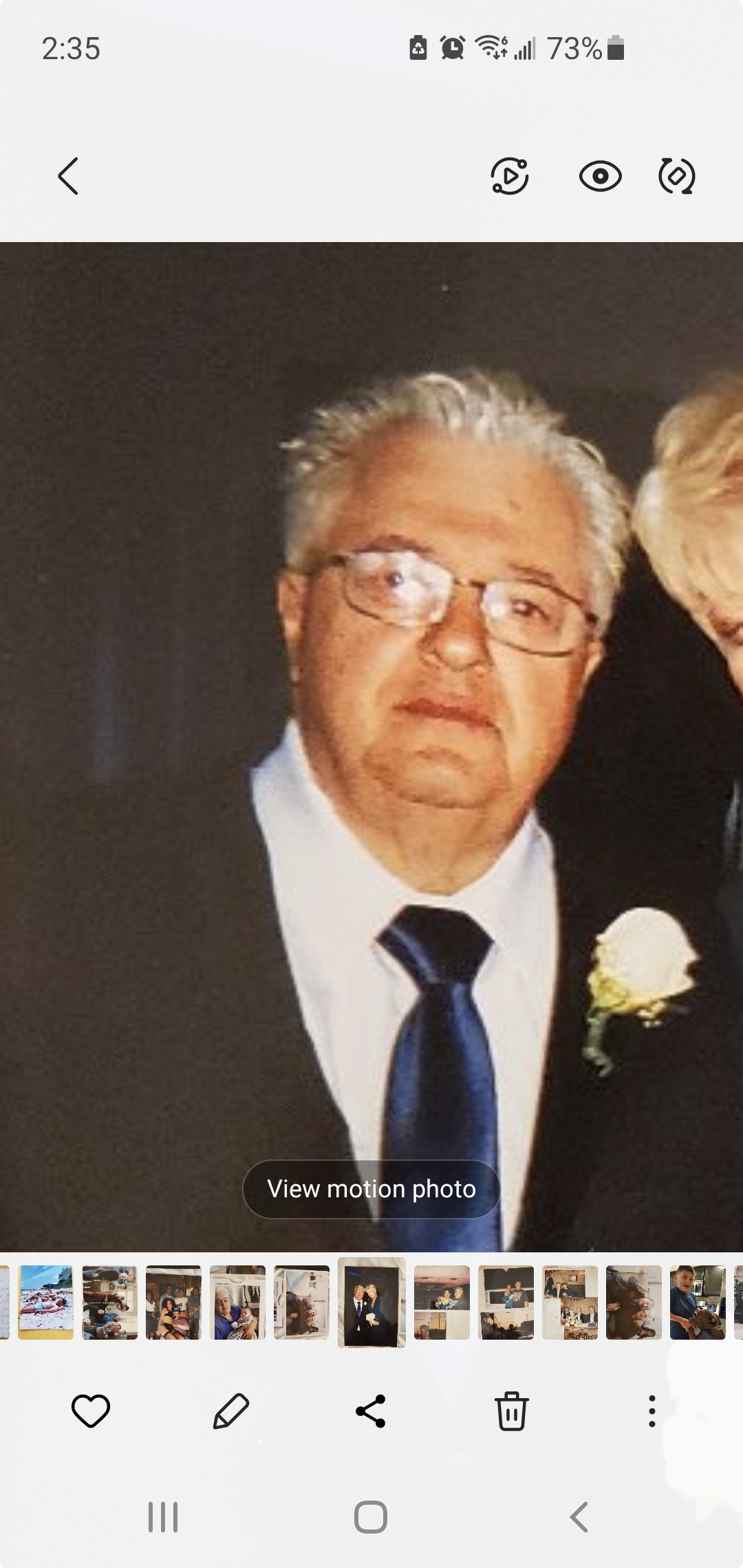
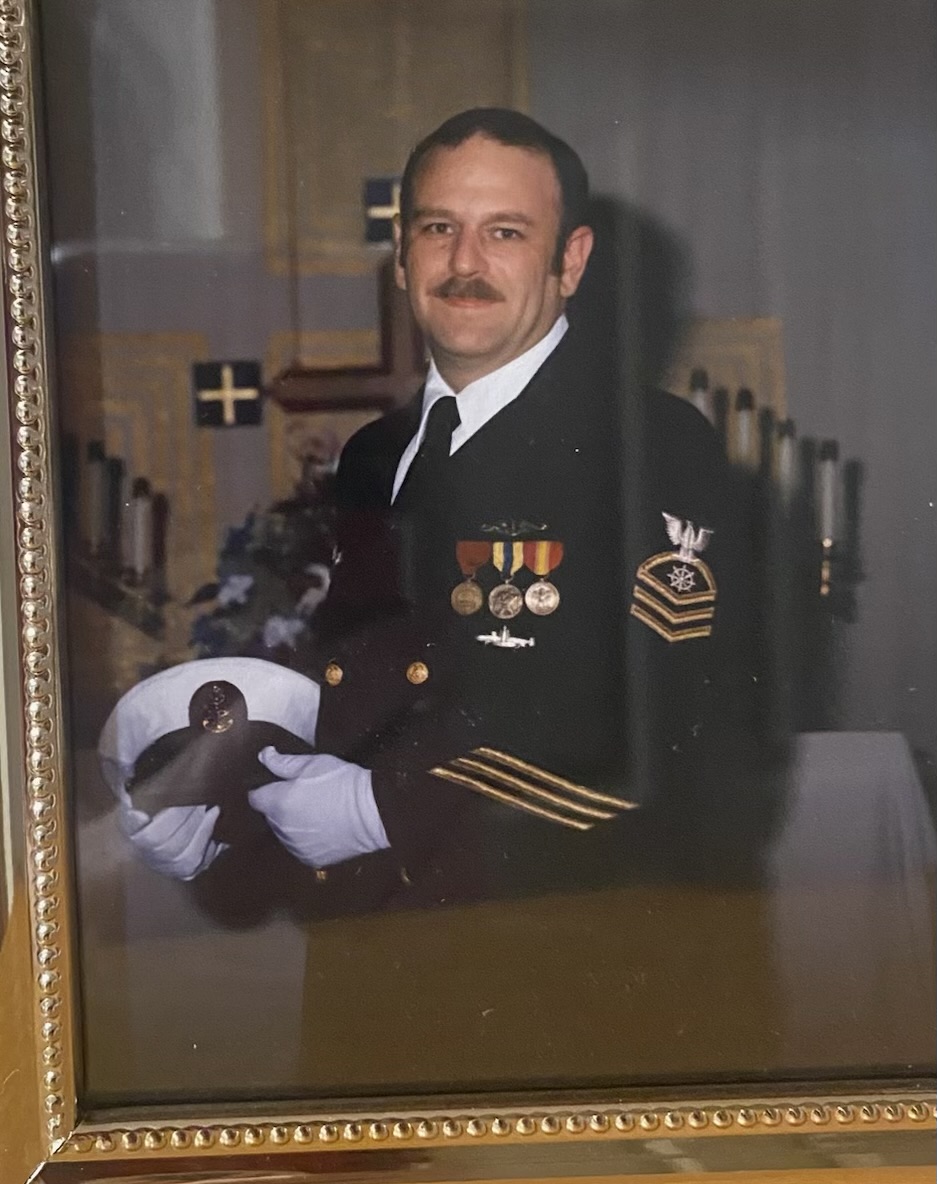
Thomas Joe Suggs
Age: 76
Location: CA
Admitted: 12/26/2022
To: Clovis Community Hospital
Murdered: 12/30/2022
Thomas Joe Suggs


My name is Blayne Johnson, and I was lucky enough to be Barbara’s daughter-in-law. I became the family advocate and spoke to the doctors and nurses during her two hospital stays in 2020, and 2021, on her behalf. I took my role very seriously since I knew she was alone in a hospital and wanted her to think about getting better.
I, along with my husband, Chris, are telling Barbara’s story. A story no loved-one should have to tell, but we hope it spreads awareness as to how our loved ones were treated during the 2020 pandemic. I have kept all my notes since that time, and I hope to recount this nightmare as accurately as possible.
Barbara was a wife, a mother, a Grammy, a sister and a friend. She was ours, and we miss her tremendously.
Barbara was diagnosed with leukemia in August, 2020, three months after her retirement. What she thought was going to be the beginning of spending more time with family and traveling, turned to be the last year of her life.
Barbara was a fighter. She battled leukemia head on; saying she was going to beat it. She had kids, a husband and grandbabies to spend time with! She fought alone and hard for over 40 days in the hospital. Her family could not be by her side, but we FaceTimed, texted and spoke all day.
When she was released from the hospital in October, she cried happy tears, seeing her husband for the first time. She was weak, but she was alive. She was able to be home, go on walks with her husband and finally hug her family. She was so happy! She still had a long road ahead and was still receiving blood platelets, but she was out of the hospital and in good spirits.
On December 17, 2020, my youngest son and I were out, and I asked if she was hungry for In-N-Out. She said she was not super hungry, but a chocolate milkshake sounded goo! So, I, of course, got her what she wanted. When we got to her house, she was tired and seemed a little out of it. She did not eat or drink much, so I knew she was not feeling well. Her nurses had been there that morning for her labs for her leukemia, so if anything were wrong, we would know.
Later that afternoon, Barbara’s oncologist called her and said she had seen her labs, and that her office was closed, so she should go to the ER for observation. She was concerned with her blood pressure. Barb was terrified to go back after her long stay, but figured she would be checked out and then would be home. She came by our house before they left and gave hugs to her son, me and her grandbabies. That would be the last time we would ever see or hug her.
Her husband took her to the ER and had to drop her off. Since this was 2020 in California, hospitals were still closed to any visitors, so you were not able to escort your loved-one inside. You simply had to drop them off.
She texted us from the ER, and said she was in a shared room with a curtain between the. I asked that she request an isolated room since she was immunocompromised, but she wasn’t moved. She was in the hallway, at one point. This was not where you want to be when you are in remission. They tested her for COVID-19, which came back negative.
They admitted her on 12/18/2020. She was having a tough time breathing and began running a fever, which is a concern in leukemia patients. They started multiple antibiotics, antivirals and steroids to try and get rid of whatever infection she had. She was again given a COVID-19 test which came back negative. They mentioned doing a bronchoscopy, but needed her blood pressure stable before they could. They tested her for Valley Fever, but that was also negative.
December 22, 2020, she was put on a bi-pap machine due to her breathing. Over the next couple of days, we spoke to her via test and FaceTimed often. She was extremely sick, but she was strong and fighting. She was supposed to have the bronchoscopy, but it was cancelled for reasons we were never told. She had waited all day for the procedure and was not able to ear. She said she was hungry and would, hopefully, get to eat soon. Poor thing was so weak and starving.
On Christmas Eve at around 4:00 or 4:30 in the morning, my husband received a FaceTime call from Barbara’s phone. She was calling with the doctor. They said they would like to do the bronchoscopy, and they needed to intubate her to do so. Immediately, my husband shook his head and said, “No, you are not going on a ventilator.” The doctor assured us she was only going to be on it for a brief time – to do the procedure and to give her lungs a little break. Barb was with the doctor and whispered, “I’ll be fine.”
The procedure was to be done that morning, and we asked that they call us to let us know she was doing after. No call came. I called around 11:30 a.m., to inquire and was told very coldly, “There was no bronchoscopy; Barbara tested positive for COVID-19, and they couldn’t do the procedure. To say we were shocked, is an understatement. Shocked, mad, confused, so many emotions. How does one get COVID-19 in a sterile hospital? We weren’t allowed in due to COVID-19… how did she suddenly have it? They had tested her on December 17, 18 and 21st, and now, suddenly, she has COVID, and she’s on a ventilator?!
Once she was diagnosed with COVID, everything got worse. Not only was she now fighting for her life on a vent, we suddenly could not talk to her. We were still able to FaceTime, and she could shake her head “yes” and “no,” but it was not the same. On Christmas, we had a family FaceTime with Barb and her sister and her family. We all prayed for her and told her she was so strong and doing great! It was a Christmas that none of us will ever forget.
We were told her ventilator was on minimal setting and that she was still on multiple antivirals and antibiotics along with steroids. During this time, she was also still getting platelets and fighting her leukemia. I had numerous conversations with the doctors and nurses, and I asked if they could try ivermectin and hydroxychloroquine. They told me those medications were not FDA approved, and they would not do it. I urged them to listen to an interview from American Front-Line Doctors, and even sent him the link. He never responded saying that he had listened to it. Our wishes from the beginning were ignored.
Over the next few days, her vent setting changed minimally. She would begin to get better, but the then she would be worse and need more support from the vent. On December, her oxygen needs had increased from 45 percent to 60 percent. She was still comfortable and communicating with the nurses. I had a call in that day to see if they would allow a family member to be with her. We knew that seeing someone and holding someone’s had would make a difference, but we were denied. The doctor at that time said they were not concerned with her oxygen settings and that a lot of people were on the vent from 2-3 weeks, so be prepared.
Although she was on the ventilator, we were still able to FaceTime and text. We called several times a day – even if it were just to see her face for a few minutes and to tell her to keep fighting. I had access to her “My Chart” account, so I was able to see what was happening throughout the day. I have a friend who is a nurse who helped me with the labs I was looking at. I was determined to help in any wasy I could, even if we were not with her.
She was given remdesivir on 12/24/20. We were not consulted. We were just told they were trying a new approach. Her vent was down to 50 percent, and her x-ray showed it was stable. During our FaceTime, I have written in my notes that she was listening to worship music and blow a lot of kisses.
She began to have issues with her kidneys, and we were told it was due to the medications she was being given. On 12/30, they took her off the medication they believed to be the cause of the issue. We were told she might need dialysis, but they were trying to manage the issue without. She was also bleeding in her feeding tube, but we were told it was no longer happening. They said this can happen when you have been on steroids and a ventilator. She was able to sit up in a chair and had physical therapy. She seemed to be doing great considering the circumstances. Slowly, she was getting better.
On 1/2/2021, Barb was still improving! They were going to try a spontaneous breathing test so she could get the vent out! We were all so excited and hopeful! We were praying her lungs were ready and asked all our friend and family for prayers! The nurse was so optimistic, which was the first time any medical professional had been with her case. Unfortunately, during the breathing test, she aspirated, and they had to stop. They had to increase her fentanyl to calm her down, but, again, the nurse was feeling good about her progress. He was hoping they would be able to try the breathing test again. He said he was confident she would off the vent by his next shift. We were hopeful.
Over the next couple of day, she was still doing good. She had physical therapy, and her vent settings were in the same range. On 1/5/21, I had a call with the doctor who advised me that her lungs were severely damaged from COVID-19. Not that it was permanent, but that the longer a patient is on a vent, the harder it is to wean them off. She said she was heading in the right direction, and she was on minimal sedation. She said to keep texting and calling her to keep her spirits up.
The same day, we had not heard from Barbara at all. We had sent texts, tried calling and we were unable to reach her. I finally was able to speak to a nurse who told me she locked herself out of her phone. This was unusual since she was always alert and able to use her phone. I asked if her fentanyl had been increased. The only thing I could think was that she was loopy and could not see the numbers on her phone. The nurse advised me, yes, her fentanyl had been increased. I told the nurse we were not comfortable with her on so much fentanyl. She told me, “We do not give the patients what we want, we give them what they need.” That did not sit well with any of us.
1/6/2021, was the beginning of the end. I received a call from a doctor on call. This was a first – someone contacting us. He said she had worsened, and her vent settings were up to 80 percent. He wanted to go over her plan and what we felt she would be comfortable with. He let us know that a social worker would be calling later that. That call came around 7:00 p.m., and the social worker told us that she was 100 percent on the vent. She was no longer breathing on her own at all. How did she take such a bad turn? We were confused and heartbroken.
The following day, we had a call with all her doctors and the social worker. They told us she would have no quality of life if she survived, and her chances of surviving were 50/50. We had a very heated call, and we voiced all our concerns. How did she get COVID-19 in a sterile environment? She was tested four (4) times during her first week. Why was she allowed to share a room with someone in the ER knowing she was immunocompromised, why was she on so much fentanyl? In the beginning she was on 50 mg, and the nurse said he was impressed. She tolerated pain so well, and now she was up to 300 mg! How would she be able to fight so drugged up! Why wasn’t more done? Why couldn’t a loved-one be with her? It could have made the difference she needed. Our concerns were met with resistance, and they took no blame. Our mom was now in a coma and drugged up and on a ventilator and nobody could answer any questions. This was the COVID-10 protocol, and she was dying.
The doctors urged us to remove the ventilator and let her body go. They could not tell how long she would survive, but it would not be long. Her husband was finally able to see her and sit with her. She looked nothing like his beautiful Barb. He even showed her picture to the nurses so they could see what she really looked like. How beautiful and healthy she was. Nobody was ready to let her go, and we continued fighting.
My husband was able to go for the evening of 1/9/21, and he was told she was not going to make it. When he got there and sat with her, he felt it wasn’t time. He could not let her go and didn’t think she was ready. He came home that night in so much pain. Not knowing if she would pass before the morning; praying, she would not. She did not. She survived the night, but the next day they called again to let us know things had gotten worse. At this point, they were only going to allow two family members. Barbara had two children and a husband. We begged for the three of them to be allowed to say goodbye. Luckily, they allowed it.
The three of them sat and listened to worship music with her. Her hair was in dreadlocks from not being brushed. Her mouth was bloodied and dry. Her teeth had shifted due to the ventilator. This is the only time they got to be with her to watch her die. Her fentanyl was up to 350 mg. The decision to remove the ventilator is one that haunts them to this day. There was so much pressure from the doctors. So many times, they said she could be brain dead. She would have to have full care if she came out of it; is this what you want?
They decide this is not how she would want to live, so they made the hardest decision they had ever made. Once they removed the vent, they sat with her. Barbara passed and took her last breath surrounded by her children and her husband. They watched a tear slide down her fact, and at that point, my husband was not sure this was the decision they should have made. She was gone.
I know this story is long, but this is Barbara’s story and I wanted to give as much detail as possible. Even now, after writing this, I know I missed so much. There is more to say, but there will always be more to say. There is not a day that goes by that we do not think of her. Our kids talk about her, we celebrate her and we include her in all special moments in our life. We miss her, but she will never be forgotten.
Filter By Category
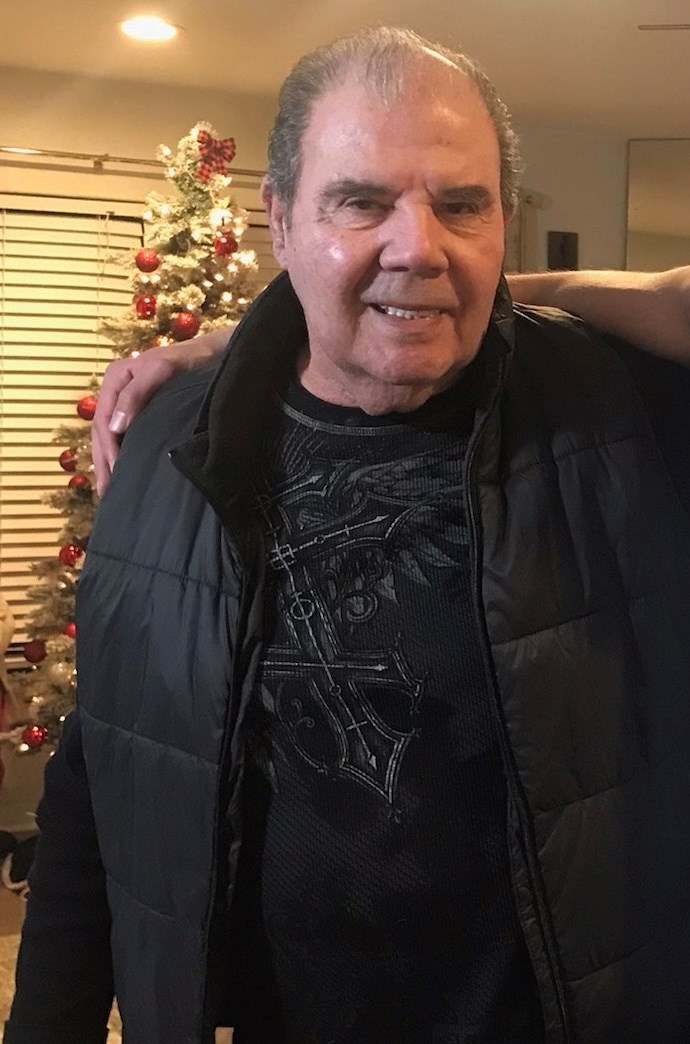
Age: 76
Location: CA
Admitted: 12/26/2022
To: Clovis Community Hospital
Murdered: 12/30/2022
Thomas Joe Suggs

Age: 56
Location: TX
Admitted: 12/25/2020
To: Baylor Scott and White All Saints Medical Center
Murdered: 02/03/2021
Ed Hodges

Age: 47
Location: MI
Admitted: 01/02/2022
To: Huron valley hospital-DMC Commerce,Mi
Murdered: 01/12/2022
Brian Pickl
Age: 76
Location: NY
Admitted: 12/26/2020
To: Montefiore St Lukes Cornwall
Murdered: 01/15/2021
Mr. Matos

Age: 58
Location: OH
Admitted: 11/21/2021
To: Aultman Hospital
Murdered: 12/06/2021
Kevin Turkall

Age: 41
Location: IA
Admitted: 01/06/2022
To: Allen Unity Hospital in Waterloo then Mercy Hospital in Des Moines
Murdered: 02/05/2022
Joshua Vandenburg

Age: 59
Location: NY
Admitted: 10/02/2021
To: Saint Catherines
Stanley j. Czarnecki

Age: 56
Location: CA
Admitted: 08/24/2021
To: Kaiser
Murdered: 09/18/2021
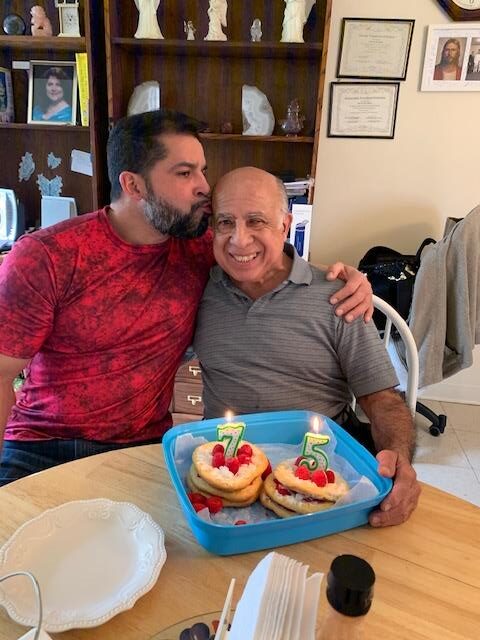
Gustavo "Gus" Enriquez
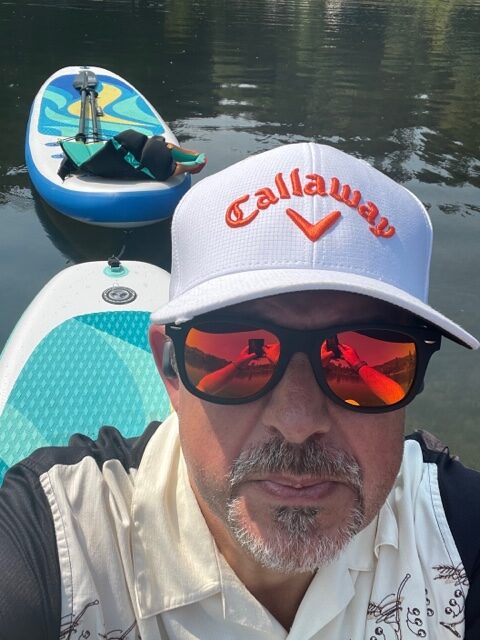
Age: 44
Location: WA
Admitted: 03/27/2021
To: Swedish Issaquah and Swedish Cherry Hill (Seattle)
Joel Finch

Age: 65
Location: MN
Admitted: 12/29/2021
To: Allina Health in Faribault, MN and transferred to Abott Northwestern in Minneapolis, MN.
Murdered: 01/10/2022
Paul Jerome Swenson

Age: 53
Location: TX
Admitted: 09/07/2021
To: Hugely Hospital
James Stuer, Jr.

Age: 44
Location: IL
Admitted: 11/21/2021
To: Riverside Medical center Kankakee
Murdered: 12/24/2021
Sara Heagle
Age: 78
Location: GA
Admitted: 04/03/2023
To: Piedmont Faytteville GA
Murdered: 04/17/2023
John Curror Fleming

Age: 65
Location: OH
Admitted: 12/15/2021
To: Lima Memorial Hospital
Murdered: 12/28/2021
Roger Shellenbarger

Age: 68
Location: CA
Admitted: 07/23/2021
To: Sharp Memorial Hospital
Murdered: 08/08/2021
David Charles Coleman
Age: 77
Location: NY
Admitted: 04/04/2021
To: White Plains Hospital
Murdered: 04/15/2021
Richard Bonfiglio

Age: 50
Location: SC
Admitted: 09/10/2021
To: Roper St Francis Mt Pleasant Hospital
Murdered: 10/13/2021
James V. Lamb, III

Age: 60
Location: MI
Admitted: 11/17/2021
To: Sparrow Hospital Ionia Michigan
Murdered: 12/13/2021
Jeffrey Jay Marshall

Age: 41
Location: AR
Admitted: 09/22/2021
To: Baptist Health
Crystal Marie Alonzo
Age: 67
Location: WA
Admitted: 10/05/2021
To: Skagit Valley Hospital, Mount Vernon, Washington
Murdered: 12/06/2021
James Christopher Rutherford

Age: 67
Location: MI
Admitted: 02/23/2022
To: St. John Ascension and ambulances to Beaumont Troy because St. John’s wasn’t equipped to handle COVID patients
Murdered: 04/02/2022
Kenneth Michael Kvasnak

Age: 73
Location: IL
Admitted: 12/10/2021
To: Riverside Medical Center
Murdered: 12/29/2021
Fred Vagt

Age: 53
Location: OH
Admitted: 01/04/2022
To: Clinton Memorial
Murdered: 01/29/2022
Todd L. Pointer

Age: 47
Location: CA
Admitted: 09/03/2021
To: Desert Valley Hospital
Murdered: 10/09/2021
Oscar Daniel Moreno
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.