
Murder by Remdesivir–Suzanne’s Story
Age: 79
Location: MN
Became sick: 02/24/2022
First sought care: 02/24/2022
Admitted: 02/24/2022
To: CentraCare Rice Memorial Hospital, Willmar, MN
Murdered: 03/18/2022
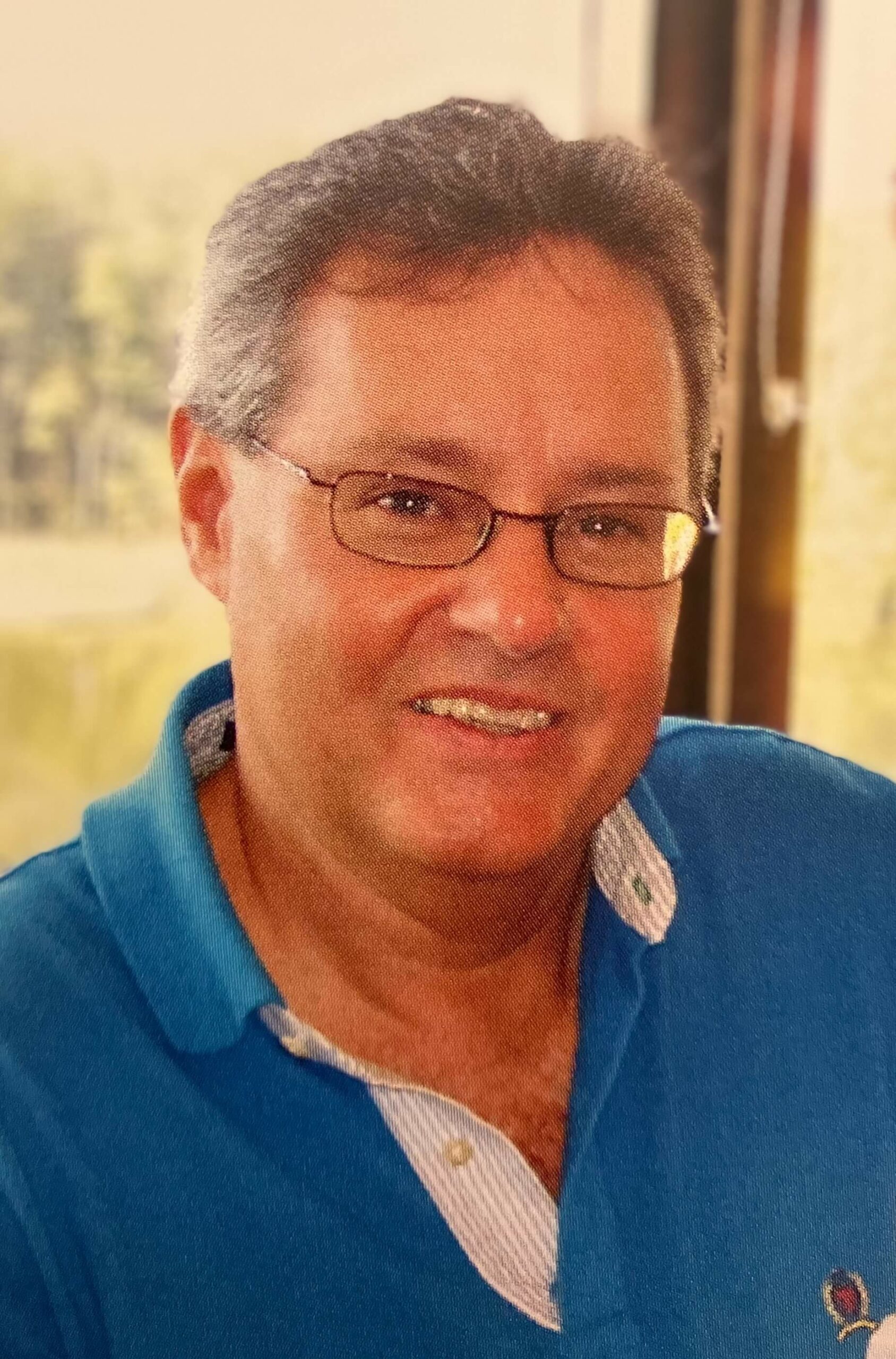
Charles Knutson


On Feb. 9th my husband wasn’t feeling well. We had all been sick for a few days but got over it quickly. I had a headache and felt like I had the flu. My husband felt the same but his lasted about a week and he just couldn’t shake it. He had chills, fever, body aches. I was giving him NyQuil and he went to bed. I thought he was nearing the end of it, when his fever started spiking to 103. I was then putting cold compresses, extra blankets, Tylenol and Robatussin for a cough & congestion. Then on the morning of Feb. 23rd, he woke up and sat on the couch but his breathing sounded funny. Just a little short of breath and he was tired and had no energy.
I told him that I didn’t know what else to do for him and that I felt like he had to go to the ER. He said fine, but he wanted to lay down and take a nap 1st. I went to the store and bought a pulse oxomotor and it was at 80. I told him we had to go to ER which was around the corner at St John’s Ascension Hospital. I pulled up to the ER, put him in a wheel chair. The registrar had me fill out an electronic form. It was not questions about COVID but it wouldn’t let me pick and choose the symptoms and he didn’t have all the symptoms. I told her that I didn’t feel comfortable with this form or feel comfortable signing it. I told her I think it’s the flu that changed to pneumonia. But, she was not hearing that! I didn’t want to fill out the paperwork or sign it. But, they wouldn’t treat him if I didn’t.
They proceeded to wheel him in the ER, I was not allowed back there. They supposedly gave him a COVID test which was maybe a min later they claimed he had COVID. They would not let me go back there with him and when I said that he has hearing aides but he doesn’t have them in and I wanted to make sure he could hear them, the registrar said “well, he can hear you just fine.” She told me to wait in the parking lot or go home and they would call me. I told her we lived around the corner and I had 2 young boys at home so I went home. They never called me.
I got a text a few hours later from my husband saying that he was in the ambulance on his way to Beaumont Troy because St. John’s was not equipped to treat COVID patients. They never called me. I called Beaumont Troy and he had not arrived yet. I called back about an hour later and he was in a room in the basement waiting for a room. He had an oxygen tube under his nose and his oxygen levels were up to 95. It was late at night by then so I told him that I would be there at 6am to pick him up and that he can discharge himself at anytime. I was in the parking garage at 6am and I texted him to tell the DR’s that he wanted to be discharged.
By that time, I had received a call from the head nurse telling me that he had to be put on a higher oxygen mask and that he was not well enough to leave the hospital. She told me that I was risking his life if I had him leave and that he would not make it to the elevator. I knew right then, that he was trapped in the hospital and they were not going to let him leave. My sister works at a home care/ Hospice facility and she gave me the phone number of one of her bosses or coordinator. I explained the situation and she said that she could set him up with in-home care with oxygen and that our insurance covered it. She was working on establishing him as a patient.
Ken’s oxygen levels never got low enough to allow the in-home care. I got a call from the head nurse and a social worker from Beaumont hospital. They asked me all kinds of questions and when I said that I was his wife the head nurse said, ”well anyone can say they are his wife.” I told them I have a marriage certificate to prove it and that we have been married for 25 years. She asked if we had any Power of Attorney or a Patient Advocate in place and I said no. We didn’t have anything. I told her I was having In-home care take care of him at home with oxygen as soon as his levels got down to 7 L or something. I should never have told her that plan. They made sure his levels never went down.
I went on-line to fill out a patient advocate form and printed it off to take it up to the hospital for him to sign. They told me that I wasn’t able to come up to the hospital because he was quarantined and that I would have to sign the paperwork in front of my husband and then he would have to sign. She then told me that he would have to authorize me to be his patient advocate and that he had not authorized me. I texted him and told him to authorize me. Which he did.
After a few days of them telling me that I was not authorized because he had not authorized me to be his patient advocate, I told the nurse to put the phone up to his mouth and to tell the nurse while I was on the phone that he approved me to be his patient advocate. Which he did. But, they still would not let me up to see him. I asked several times to talk to the Dr. Every nurse I talked to said they would give him the message, they even typed it in his chart. I never got a call from the Dr. finally,(not sure how many days later) I got a call from the Dr. He told me that I was not allowed to see my husband because he was quarantined even though he admitted that my husband no longer had COVID.
I said that the CDC stated that after 5 days from becoming ill, he was no longer infected and did not have to quarantine. He said that I couldn’t come up because my husband was on oxygen. Which never made sense to me. I said that I would put any PPE on and do whatever I needed to do. He refused. I had to wait 20 days before I could go see him. The day that the Dr called me to tell me that I could come up, I was told that we could have 3 people but one at a time at bed-side. We had to go through security, we had to wear a mask, and that we had to be family members only.
As my brother-in-law, sister-in-law and I were walking down the hallway to see my husband we were stopped by a nurse who proceeded to tell us that when my husband was trying to urinate at bed-side, he took his oxygen mask off and his oxygen level dropped to 40. He turned blue and unresponsive and that she had to shove the mask back on. He was stable she said. And she allowed me to go in. Another nurse was in the room, she told me the same thing.. that he was blue and unresponsive and that they had to put the oxygen mask back on him. Then she said that his chart says DNR so they didn’t have to put the mask on.
I walked up to my husband and got close to his ear and said, “Ken, you mean to tell me that if something happens you do not want to be resuscitated?” He said “ I never said that” I was livid! The day I could finally go see my husband and he almost died before I got to the room. I told that nurse that I am not leaving until you get someone down here to change his chart. And she did. The Dr. came into the room and we were talking about Kens condition. I could tell that breathing was hard for him and that it was difficult to talk with the mask on. His lungs were working hard and the Dr. even pointed it out to me.
He said that he cannot last much longer on the Bi-pap oxygen mask because his body is working so hard to breathe. It’s like he’s been running a marathon. I asked what his options were. He told me he would die on this level of oxygen or he could go the next step which is the ventilator. He would most likely die on the ventilator. I said, “So, my options are that he will die with this oxygen or he will die on the vent. Either way he will die.” He said , “Yes, that’s why you should have taken COVID precautions”.
I was so mad and upset that he would have the nerve to say that to me. I felt cornered. The only way to help my husband was to put him on the vent so that his body could rest and maybe he would have a fighting chance. I told the Dr that my step-kids were about 3 hours away and that they needed to see their dad before we do the procedure. He told me not to wait too long. I got the older kids here as soon as they could which I believe was the next day.
We requested a family meeting with the Dr. and his team because we had all kinds of questions. My daughter-in-law is a registered nurse and she researched different cases and treatments and had a list of questions to ask. When we all got to the hospital (my husband’s brother, his wife, my step-son, his wife, my two younger boys. My step daughter came later). We asked all kinds of questions to the Dr and his team and the Dr. shot down every one of our questions and solutions saying that none of it would work.
He then said to my daughter-in-law (the nurse) “Have you seen the news? Do you know what COVID is?” Personally, he was so arrogant that I don’t think he liked the fact that we were questioning him and his form of treatment in front of his team of DR’s and that we were questioning his authority. I then had everyone leave the room and I talked to my husband alone. I knew he was scared and confused and he didn’t know what to do and he just wanted to go home and he couldn’t believe how all this could have happened.
I told him that the only thing that we can do is to put him on the ventilator and I explained that he may die but that his body needed to rest and I wanted to give his body that rest so he can fight this. I keep hearing his voice in my head telling me “I want to live!” It haunts me. He agreed to go on the vent, “Just do it” he said. I poured my heart out to him telling him how much I loved him, he was such a great dad & husband. How he was a great provider. My one true love.
I then let the other family members in to see him one by one. Even my two young boys. The Dr & nurse tried to stop me but I got in the Dr’s face and told him that we are not doing these stupid rules today. That my boys are gonna say what they need to say to their dad and he is not stopping it. He told the nurse who was standing right there to allow us the time we need. He left and she kept telling me we had 10 min. How can you say all the things that you need to say in 10 min? They were clearly pushing us to get him on that ventilator.
After he had been out on the ventilator, the Dr’s would tell me that he only could be on it for about 12 days. Then, bacteria would set in around the tube. I asked what the next step would be. They said a Trachial tube but that he didn’t qualify because on the ventilator his oxygen levels were pretty much at the highest and if they could lower the oxygen, get him less dependent on the oxygen, they could do the procedure. But, at that time, he wouldn’t survive the procedure. The specialist who was controlling the oxygen levels on the ventilator tried to reduce the oxygen as it got closer to the 12 day deadline. But he would reduce it a lot like every hour it seemed in one day. It wasn’t gradual at all. Which I found to be weird. Then he had to increase it to a high level again.
While he was on the ventilator, I came up to his room to sit with him, talk to him, sing to him, brush his hair. The nurses didn’t like me too well because I would tell them he stunk & needed a bath or tell them to take a shampoo cap and wash his hair. They never did. Only once did I witness a bath with what looked like a baby wipe. He was paralyzed and on a ventilator. It was hard to wash him cause when they moved him, his oxygen levels dropped. As it got closer to the 12 days, the Dr’s kept pressuring me to take him off the ventilator. Finally, in a meeting with a female Dr and the head of the ICU, I told them both that I am not taking him off the ventilator until his body tells me that it can’t fight anymore and that it’s shutting down.
I think it was about 10 days when his kidneys were starting to shut down. He had developed blood clots, an infection of some kind, and I think he was turning septic. He was looking discolored. His lungs were filling up with fluid and it was starting to back up into his throat. You could just tell it was time to let go. The hardest thing I have ever had to do was consent to take him off the ventilator. They called in a specialist to take him off the paralytic which they said was “inhumane” to take him off the ventilator with it on. Like any of this was humane! So wrong. We were all standing around him when he passed, except my youngest boys who were in the waiting room just down the hall. I couldn’t let them see that. It was a lot for all of us adults to take in.
Filter By Category

Age: 79
Location: MN
Became sick: 02/24/2022
First sought care: 02/24/2022
Admitted: 02/24/2022
To: CentraCare Rice Memorial Hospital, Willmar, MN
Murdered: 03/18/2022
Charles Knutson

Age: 62
Location: AK
Became sick: 08/22/2021
First sought care: 08/25/2021
Admitted: 08/31/2021
To: Providence
Murdered: 09/15/2021
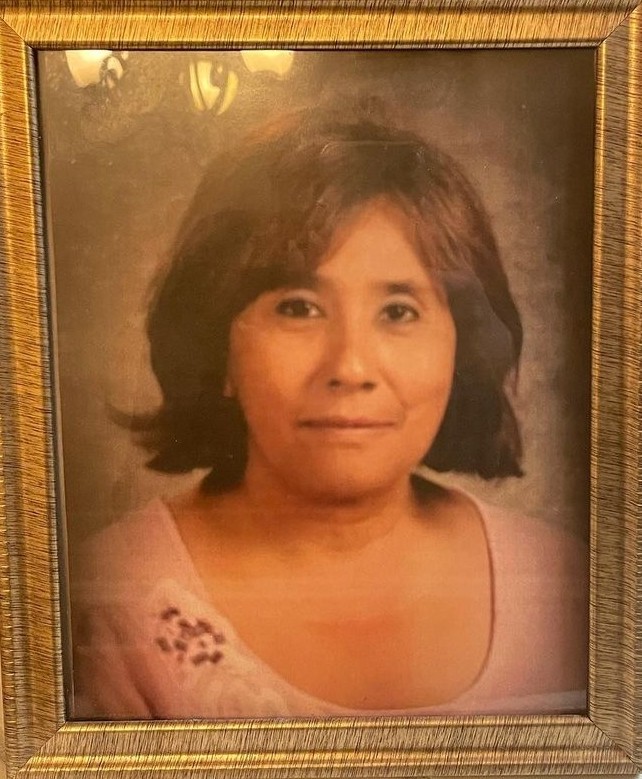
Fannie Downes

Age: 67
Location: IN
Became sick: 10/09/2021
First sought care: 10/11/2021
Admitted: 10/17/2021
To: St. Francis Lafayette
Murdered: 01/19/2022
Marsha Walker

Age: 48
Location: CA
Became sick: 07/30/2021
First sought care: 08/04/2021
Admitted: 08/04/2021
To: Clovis Community Medical Center
Murdered: 09/28/2021
Guadalupe "Lupe" Espinoza

Age: 66
Location: FL
Became sick: 08/06/2021
First sought care: 08/14/2021
Admitted: 08/14/2021
To: Lake City VA Hospital and Malcolm Randal VA Medical Center
Murdered: 09/02/2021
John W Shannon

Location: IL
Became sick: 12/21/2021
First sought care: 12/22/2021
Admitted: 12/22/2021
To: Local Medical Center
Murdered: 12/29/2021
Mary Lou Fosnaugh

Age: 35
Location: TX
Became sick: 08/20/2021
First sought care: 08/26/2021
Admitted: 08/29/2021
To: Azle Memorial Hospital
Murdered: 09/14/2021
Jennifer Nichole Smith Mason

Age: 64
Location: TX
Became sick: 01/03/2022
First sought care: 01/10/2022
Admitted: 01/28/2022
To: Medical City Alliance
Murdered: 02/21/2022
Don Truman Taylor

Age: 66
Location: MT
Became sick: 10/11/2021
First sought care: 10/19/2021
Admitted: 10/24/2021
To: Logan Health Kalispell and Whitefish
Murdered: 11/02/2021
William Rowson

Age: 57
Location: PA
Became sick: 10/19/2021
First sought care: 10/25/2021
Admitted: 10/25/2021
To: Mount Nittany Hospital and Geisinger Hospital
Murdered: 11/26/2021
Dennis Donald Peters

Age: 51
Location: NJ
Became sick: 09/02/2021
First sought care: 09/05/2021
Admitted: 09/05/2021
To: Shores Memorial , NJ
Murdered: 09/09/2021
Chuck Hammel

Age: 62
Location: MO
Became sick: 07/05/2021
First sought care: 07/09/2021
Admitted: 07/16/2021
To: Liberty Hospital, Liberty MO
Murdered: 07/24/2021
D. Keith Carpenter

Age: 59
Location: NC
Became sick: 10/06/2021
First sought care: 10/08/2021
Admitted: 10/08/2021
To: First Health Montgomery Memorial Hospital (Zip Code: 27371); First Health Richmond Memorial Hospital (Zip Code: 28379)
Murdered: 10/18/2021
John Joseph Adams

Age: 45
Location: CA
Became sick: 07/20/2021
First sought care: 07/24/2021
Admitted: 07/26/2021
To: Little Company of Mary
Murdered: 08/08/2021
Philip Martinez

Age: 72
Location: MO
Became sick: 10/22/2020
First sought care: 10/26/2020
Admitted: 10/26/2020
To: Southeast Hospital Cape Girardeau
Murdered: 11/12/2020
Patsy Young

Age: 56
Location: WY
Became sick: 09/30/2021
First sought care: 10/07/2021
Admitted: 10/16/2021
To: Wyoming Medical Center
Murdered: 11/03/2021
Richard “Zak” Szekely

Age: 47
Location: WI
Became sick: 09/14/2021
First sought care: 09/21/2021
Admitted: 09/28/2021
To: New London Hospital and Froedtert Hospital in Milwaukee
Murdered: 10/28/2021
Jeff Kozlovsky

Age: 65
Location: WI
Became sick: 11/09/2021
First sought care: 11/16/2021
Admitted: 11/16/2021
To: Appleton Medical Center
Murdered: 12/14/2021
Barbara Lowney

Age: 42
Location: AZ
Became sick: 08/15/2021
First sought care: 08/19/2021
Admitted: 08/19/2021
To: Banner Health
Murdered: 08/20/2021
Olivia Muralles
Age: 67
Location: CA
Became sick: 07/20/2021
First sought care: 07/28/2021
Admitted: 07/28/2021
To: Clovis Community Hospital
Murdered: 08/31/2021
Angie Murrieta

Age: 39
Location: OR
Became sick: 10/08/2021
First sought care: 10/20/2021
Admitted: 10/21/2021
To: Providence St Vincent
Murdered: 10/30/2021
Andrew Amparan

Age: 77
Location: FL
Became sick: 10/06/2020
First sought care: 10/08/2020
Admitted: 10/09/2020
To: Countryside Hospital
Murdered: 10/29/2020
Gerald ( Gary ) Russell

Age: 67
Location: IA
Became sick: 05/24/2021
First sought care: 05/24/2021
Admitted: 05/28/2021
To: St Lukes Hospital in Cedar Rapids, IA
Murdered: 06/27/2021
Ronald Pettit

Age: 80
Location: PA
Became sick: 12/24/2021
First sought care: 12/28/2021
Admitted: 12/28/2021
To: Phoenixville Hospital
Murdered: 01/04/2022
Eva Hicks
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.