
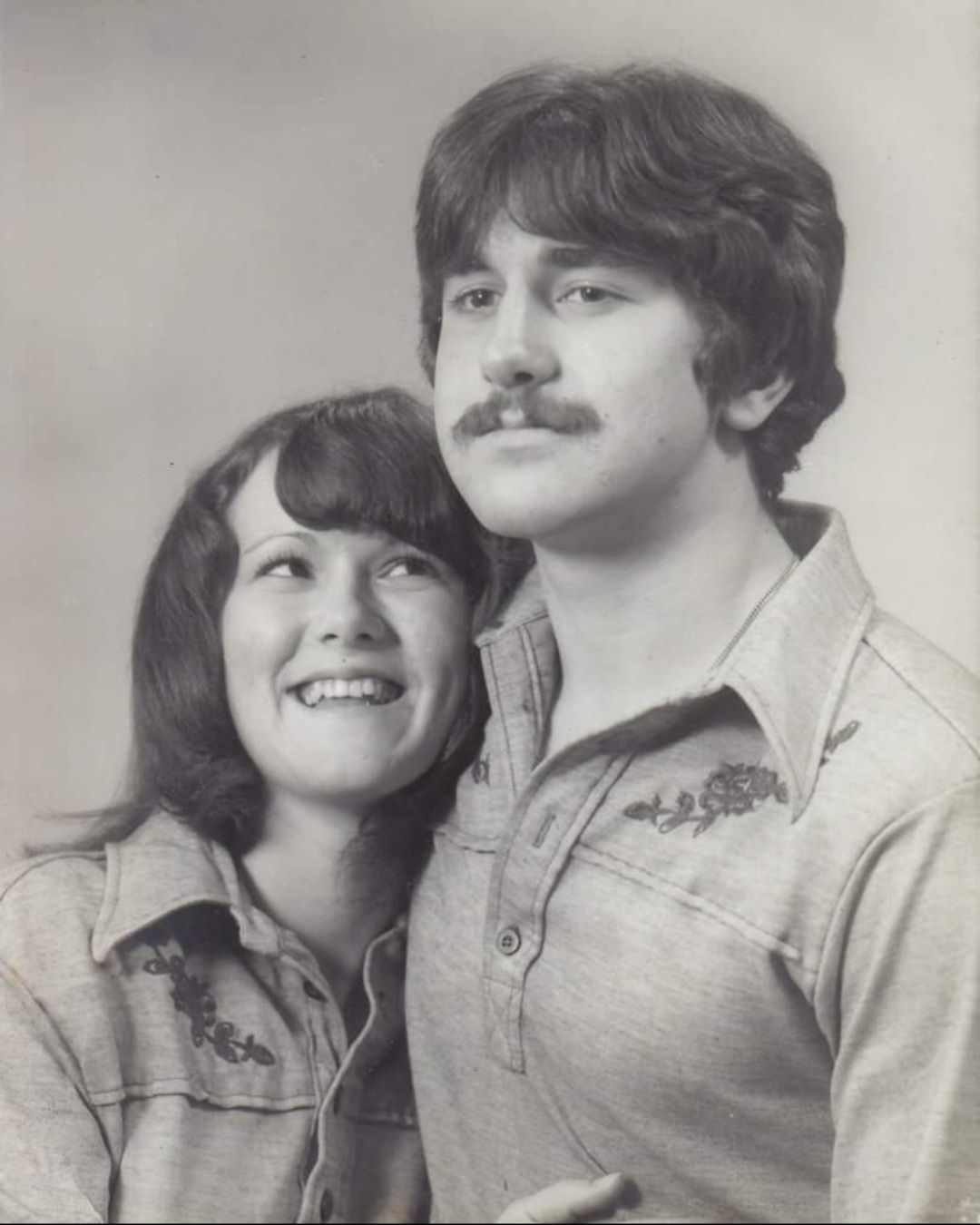
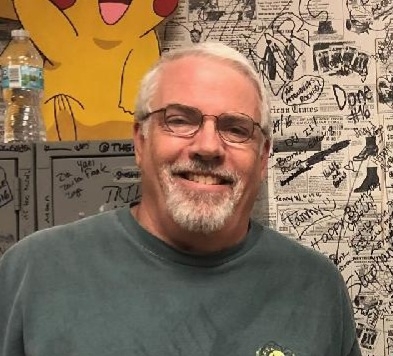
Terry Wisdom Jr. – Husband, Father, Pops, Veteran!
Age: 54
Location: SC
Admitted: 08/28/2021
To: Coastal Carolina was the first hospital I took him to on Saturday morning; Beaufort Memorial on Saturday evening.
Murdered: 09/08/2021
Terry Wisdom Jr.


Response time to patient calls was very slow. Staff very "unconcerned" with my husband's needs. Depending on the staff assigned to the room, this could vary for better or for worse.
July 5, 2021
Health and Human Services Commission
Complaint and Incident Intake
Mail Code E-249
P.O. Box 149030
Austin, TX 78714
To Whom It May Concern:
I am writing this letter to express my utmost concern and grave disappointment for the care my husband, Nicholas Passe, received while admitted to Cedar Park Regional Hospital from June 17, 2021 to June 26, 2021. He was, unfortunately, admitted with SARS-CoV-2 related pneumonia with Severe acute respiratory syndrome CoV-2. In addition to the poor care my husband was given, the hospital staff fell woefully short in adequately communicating with family and providing updates on patient status given that he was isolated and visitation was not allowed by family.
I am not only the concerned spouse in this situation but I am a Medical Surgical RN of 5 years and a certified Family Nurse Practitioner with 15 years of Family Medicine experience and currently practicing as a Rheumatology Nurse Practitioner. All this to say that I am acutely aware of clinical guidelines, policies, and procedures when it comes to in-patient care and expectations that family have when it comes to caring for their loved one.
During his admission, my husband was given the appropriate medical care in that he received medications according to evidenced based COVID guidelines. I am not disputing the medical care in any way and I am thankful that his condition improved because of these interventions.
However, when a patient is isolated from literally everyone, including the medical staff, and they are critically ill, limiting their mental capacity to process information and formulate questions, this results in a very vulnerable patient both medically and mentally. With the lack of a patient advocate, ie, family, the care of and communication with the patient and family is absolutely vital and should be efficient and continuous.
I was not allowed in the ER holding bay with my husband before his admission due to his COVID positive status, despite being fully vaccinated and wearing a mask. It took hours to get a call from the admitting physician, Dr. Reddy, just to get basic updates on status and plan of care. My husband is not medically inclined at all, like most patients, and does not understand medical jargon so getting information from him about oxygen saturations, vital signs, lab work, and plan of care was menial at best.
He was finally moved to the Medical Surgical floor later in the evening on June 17 and I was able to bring him some fresh clothes and dinner. Again, I was not allowed to see him even though he is on a floor with nothing but COVID patients and I am fully vaccinated. I was told a nurse would call me with his status at some point that evening. I never heard from a nurse but my husband sounded fine and comfortable so I let it be.
Over the next days, the 18th and 19th, I texted my husband often and used Face Time to see him in the evening to try and get information about his status: vitals, medications, O2 saturation and amount of supplemental oxygen he was getting. Again, I got limited information from him other than his chest was hurting, it was tight, he was coughing quite a bit and he had increasing diarrhea. I would ask him often if he was letting his nurse know and he would tell me, “well, they don’t really come in.” Still, no call from a nurse or physician.
By the evening of Sunday, June 20th, I knew something was not right. I was getting one word answers from my husband, he was very short with me and he was clearly frustrated. I asked him if his bed sheets had been changed and if he was offered anything to take a shower with because, again, he was having diarrhea and it was difficult to get to the bathroom with his oxygen and waiting on someone to come in to help him. Again, he told me “NO! THEY DON’T COME IN OFTEN.” I Face Timed him at 10 PM and could tell that his oxygen supplementation was higher than the 3 1/2L he was admitted on because I could hear it blowing loudly. I asked him to press the call light to get the RN to come in the room so I could talk to her. I heard the nurses station ask him what he needed and said they would send the nurse in.
By 10:30, while still on Face Time, no one had come in. I asked him to press the button again. By 11 PM that night, the RN still had not come in and my husband had hung up with me and would not respond back by text. I was worried and not happy at this point.
I texted my husband on my way to work on June 21 at 7:12 AM and again at 8:17 because I hadn’t heard anything. He finally responded with “oxygen low.” I followed with “how low?” and got “86%” and that he was on 6-8L of O2 depending on his readings with the respiratory therapist came in. Again, I was prying for anything I could get in terms of vitals but Nicholas would provide limited information. By 9:25 I got a text saying that the physician had been in and she was going to order another CT scan because his O2 needs were higher despite the current treatment. He tells me she is going to call me. By noon, I finished with my morning clinic and still had not heard from the physician. By this time I am angry. I call the Med/Surg floor and ask to speak to my husband’s nurse.
Luckily, the person on the other end of the phone happened to be my husband’s nurse. Unfortunately for her, I let her have it. I expressed angrily my frustration with the lack of human care for my husband and the lack of communication with family and that I was in utter disbelief that his status has changed so dramatically and not a single call from the nursing staff or physician taking care of him. She apologizes and responds “I am so sorry. I thought you had been getting calls.” She informs me that Nicholas is being moved the critical care unit because of higher oxygen demands and declining status. At this point, I could do nothing more than to break down in tears from fear and days of frustration. She assures me she will have the hospitalist call me with an update and that my husband was being taken down to radiology for a CT scan.
Finally, at 1:20, I get a call from the physician with an update and that he would be receiving a new medication called tocilizumab after he was moved. I, again, voiced my frustration with the lack of communication and gave her my perspective of my husband’s status including the lack of human care and his declining mental health, and she responds, “well, are your texting and calling him” and “he seems fine to me when I talk to him.” She dismisses my concerns and tells me Nicholas’s new physician will call once they have assessed him.
He is moved to his new room by 2:30 and I did get a call from his nurse at that time giving me an update. I had inquired about seeing my husband face to face because, at this point, I am not convinced that this hospital is taking adequate care of him and I need to see him.
The nurse from the Medical Surgical floor told me she would inquire about getting permission for me to see Nicholas. Once he got moved, the CCU RN knew nothing about this. By 5:45 that evening, the Infectious Disease physician, Dr Le, called me and talked with me for more than 30 minutes. She was the only provider that listened to me, answered my specific questions, and gave me specific answers. She was very positive that Nicholas would improve after one dose of tocilizumab and she told me how she anticipated his CCU stay would progress and where he needed to be status wise in order to get released home. I voiced my concern that he was depressed due to the lack of human care and almost a week of total isolation and she was very receptive to this. She cited known studies with acute depression and COVID related in-hospital isolation. She would address this. I felt a tremendous relief from talking with her. She told me she would call me daily in the evening with updates. She is the only medical provider that kept her word.
The next morning before work, I text Nicholas for status update and to find out if he got the new medication. He says, “they gave me something.” I didn’t bother to press this issue because I assumed I would get a status update from his RN at some point. Later in the morning, I checked in with him via text asking for status update (vitals, O2 sats, heart rate) and he responds, “I can’t see it [the monitor}”. The monitor is turned away from him facing the glass to the hallway. Again, I am frustrated because as a floor nurse I would tell my patients their blood pressure, heart rate, and oxygen saturation numbers. I would tell them what medication was being administered and what it was for. I am thoroughly frustrated that I cannot get this basic information from my husband who is in the CCU where each nurse has one to two patients.
On my home from work that day, I decided to bring Nicholas dinner and I wanted to meet the staff personally since, again, I had not gotten a call from anyone that day except the Infectious Disease provider. I happened to be on Face Time with Nicholas that afternoon when she met with him. virtually. I had not heard from the pulmonary specialist or the RN taking care of him. When I arrived on the unit, I was nicely greeted and they volunteered to take him the food I brought but, again, told me that I could not see him. I calmly told them “I will take my husband his food this evening and I will not leave until I see him.” The unit clerk excused herself to get the ICU manager, Alyson Albion, MSN, RN, CCRN. Alyson asked what she could do for me and then calmly took me aside in a conference room and listened to the current situation, my concern for the lack of adequate human care and the anemic communication.
She was genuinely concerned with what she heard and she empathized with how I was feeling. She had a clear understanding of hospital protocol with COVID when it comes to isolation and visitor policy but she also understood that I was fully vaccinated, I was very familiar with PPE and how to don while interacting with an isolated patient and she made the executive decision to let me see my husband after six days of a complete nightmare. She made a few calls and permission was granted. I got to see my husband, I gave him a hug, held his hands, and got a sense of how he looked. The look in my husband’s eyes when he saw me enter the room is one I will never forget. His face lit up, his eyes widened, and a sense of relief came over him. Before I left, she assured me that Nicholas would get what he needed for a sponge bath and his bed would be changed daily.
On June 23rd, Nicholas tells me that the pulmonologist was in around 10:15 and they were planning on moving him out of CCU on the 24th. Nicholas texts me “I guess I’m still here again today even though I feel better.” I did not get a call from the pulmonologist that day and Nick still cannot tell where is O2 is at or what his sats are. At 4:45, I finally ask him to take a picture of the machine his oxygen is hooked up to so I can see the amount of oxygen. He sends me picture and I can see that he is still on a large amount of oxygen (20 LMP with 40% oxygen). Later that evening, the Infectious disease provider calls me with update. She tells me Nicholas is doing much better and he should be getting out of CCU soon. I told her I still hadn’t spoken with the pulmonologist and she says she will work on this for me. Later that evening, I get a call from the pulmonologists PA with an update. He asks me what he can do for me and I responded, “You can help me get my husband out of this hospital.” He replies, “I’ll see what I can do.”
On June 24th, Nicholas continues to tell me that he his feeling better and he isn’t sure why his oxygen supplementation is still so high. The pulmonologist comes in around 10 and Nicholas texts me “Doesn’t sound like he’s budging on letting me out of here. I told him to call you.” Finally, a little after 10 AM, Dr Soubra, the pulmonologist calls me with the ICU manager on the line as well. This is the first time I have spoken to him since Nicholas was moved to the ICU June 21st…I asked him why the oxygen was not being tapered at this time with the report from the Infectious Disease provider being so positive and Nicholas’s report that he was feeling much better. Dr Soubra felt he was still needing too much oxygen and it was not safe to move him out of CCU but they would start to taper the oxygen today to see how he was doing.
I, again, inquired about getting in to see Nicholas again seeing as though they were going to keep him at least another 2-3 days. I checked in with Nicholas around 1 pm and asked if the oxygen has been tapered down and he texts “this hasn’t budged all day. I just unplugged everything and walked around for about 15 min.” At 1:36 I got a call from the ICU manager, Alyson, and she informed me that I was given permission to see my husband daily for 15 minutes. And, they caught Nicholas walking around without his oxygen. I told her that his oxygen hadn’t been tapered and he is getting frustrated with this not happening because if it doesn’t get lowered he doesn’t go home. She assures me the oxygen is being tapered and that he must follow the orders. I texted back and told him to “behave” and he writes back “I’m gonna keep doing it every hour. They don’t even notice. Curtains are drawn. They don’t even see me detach and walk around.” I tell him that the ICU manager told me he was at 25 LPM at 50% oxygen. I tell him that if the percentage goes up any further, they will have to use mechanical ventilation. He, again, tells me, he doesn’t understand why because he doesn’t feel he is that short of breath at all. He feels they are giving him too much. I go see him later that evening and nothing has changed, his O2 level reading on the machine or his physical status. He is feeling much better.
On the morning of June 25th, I check in with Nick and all is the same. He is tired because he didn’t sleep well but feels fine otherwise. He is getting anxious now and is asking when he can leave. I put a call into Alyson at 8:00 AM to find out what is going on. She promptly returns my call and after inquiring when we might be able to get Nick out, her tone changes with me and she becomes quite stern. She tells me his oxygen requirements are critical and at any point he could require mechanical ventilation. She tells me that there is nothing more she can do and that I really should stop pressing to get Nicholas released. In addition, she tells me that Nicholas keeps getting up out of bed without asking for help and he needs to call for help. I tell her that I will talk to him but the fact that he is doing things on his own should be a good thing. Again, his perception, and my perception, of his current status is very different than what she is relaying to me. I start to doubt what is going on and start to feel that he is more critical than I think.
By 9:45 that same morning I get a text from Nicholas reading “gonna move me out of ICU.” I reply back “Really? I am confused.” I check in with him again around 11:50 and he says he is still waiting on a room but that his oxygen keeps getting lowered as they said it would the day before. I ask him to take a picture of the vital screen and tell him “I am sooooooo confused by how quick this is happening now.” His O2 sat is at 95% with heart rate of 100 bpm and he has been moved from High Frequency Nasal Oxygenation to a regular humidified oxygenation at 10 LPM. The CCU RN, Alex, calls to give me an update and let me know that Nicholas has been very motivated and they are moving him back to Med/Surg unit. By 1:30 that afternoon, he is moved to Med/Surg.
Nicholas is elated to be out of CCU but is more persistent about when he can come home. I spoke with Dr Le, the Infectious Disease, around 7 PM and she felt Nick was doing well and he should be able to go home. She didn’t see any reason for him to be still be there. When she talked to him, he was down to 3 1/2 LPM. At this point, it is already too late and the Med Sure hospitalist will not be rounding until morning. So, I just left it at that. I told Nicholas to talk with his RN to have them start working on home 02 orders so the case manager can get this taken care of by his anticipated discharge the next day.
On June 26th, I text Nicholas at 8 AM and he reports he is fine and he is ready to leave. He asks me to come up there and get discharge going. He reports he hardly saw anyone in the way of nursing staff or RT. He had his vitals checked twice but didn’t have blood work drawn despite an elevated white count at 23,000 the day before and an increased ferritin. By 10 AM, he tells me still no hospitalist. I call up to talk to his nurse but she cannot come to the phone. She calls me back an hour later and I ask her to page the provider. I let her know that he really wants to leave and anything she can do to expedite this would be appreciated.
At 11 AM, I take Nicholas lunch because he didn’t order thinking he would be discharged. At noon, I arrive, still no discharge orders. Finally, a little after 1 PM, the hospitalist arrives, gives very little information in terms of discharge other than to follow-up with PCP and take it easy. In addition, she says she sent prescriptions in for a cough medication and a medication called escitalopram, which is an anti-depressant. I asked her about this because Nicholas never mentioned this being started and no one told me he was started on this. She says, “well, he doesn’t have to pick it up if he doesn’t want to.” She says he still cannot go because his home oxygen order is not complete yet. She says it will be another couple of hours…
By 3 PM, I inquire myself about the oxygen order. The RN assures me that the case manager is working on this. He says it should be delivered to hospital by 5 PM. Nicholas is becoming irritated and angry and is getting hungry. At 5:15 the RN comes in and says the respiratory company just arrived to drop the oxygen off and would be coming in to go over things with us. After thirty more minutes, no one has come in. I saw the oxygen outside the door thirty minutes prior but no one has come in. I go out to check and the oxygen is gone. I call the nurse again. She apologizes for the wait and takes care of her discharge part. She has Nicholas sign papers and I ask “where is the oxygen?” She replies “What? I thought he was already here and talked to you all.” She leaves the room very confused and 15 minutes later her medical assistant walks in with the oxygen concentrator and the portal O2 and says she found it in a storage closet. At 7 pm that evening, I finally leave with Nichols in tow, irritated, tired and hungry.
In summary, this was a very long, frustrating, painful nine days for my husband and myself alike. From the lack of the most basic human care, to the feeling of isolation and depression, to the unacceptable deficient communication there was so much wrong on so many different levels. My purpose in summarizing this hospital stay is to bring awareness of the suboptimal care this hospital provided, the amount of advocacy I had to do for basic information despite working full time and caring for my family in my husband’s absence and the inefficiencies in discharge planning. My hope is that protocols can be updated and COVID restrictions can be changed according to recent data and the fact that the vaccine has been widely distributed and patients no longer need to be isolated in such a way. My husband’s isolation did not help in his recovery nor did it provide me with the assurance he was getting the best care available and it certainly did not help him mentally deal with this hospitalization in a healthy manner. I implore you to investigate this further and mandate that this hospital take a closer look at their touted “Human Care.”
Respectfully,
Megan M Passe
Filter By Category

Age: 54
Location: SC
Admitted: 08/28/2021
To: Coastal Carolina was the first hospital I took him to on Saturday morning; Beaufort Memorial on Saturday evening.
Murdered: 09/08/2021
Terry Wisdom Jr.

Age: 60
Location: TX
Admitted: 09/05/2021
To: Decaunter and Jacksboro
Murdered: 09/08/2021
Walter Henry

Age: 73
Location: NY
Admitted: 04/09/2021
To: Strong Memorial Hospital
Diane K. Corby
Age: 64
Location: TX
Admitted: 08/03/2021
To: Texoma medical center / Texoma Med Center Bonham
Murdered: 08/09/2021
Gerrie Burr

Age: 18
Location: OK
Admitted: 11/09/2022
To: St. Francis
Murdered: 11/09/2022
Trista Deane' Martin

Age: 64
Location: IN
Admitted: 08/20/2021
To: St Marys /Ascension St. Vincent
Murdered: 09/20/2021
Carla Masterson

Age: 70
Location: CA
Admitted: 12/10/2020
To: Mission Community Hospital
Murdered: 01/11/2021
Vazgen Madatyan

Age: 23
Location: FL
Admitted: 07/30/2021
To: Health First Viera Hospital
Brice Bowman

Age: 61
Location: CA
Admitted: 08/01/2021
To: Corona Regional and Kindred Rancho Cucamonga
Murdered: 08/17/2021
Edward H Hamlin III

Age: 84
Location: MI
Admitted: 12/29/2021
To: Bronson Methodist
Murdered: 01/08/2022
Andrew Columbus Campbell Sr

Age: 62
Location: CA
Admitted: 08/09/2021
To: Corona Regional , Corona CA
Murdered: 08/26/2021
Roberto Chavez

Age: 49
Location: GA
Admitted: 08/17/2021
To: Kennestone
Murdered: 09/01/2021
Kevin Wilson

Age: 64
Location: TX
Admitted: 09/11/2021
To: John Peter Smith Hospital and THR Arlington Memorial
Murdered: 09/27/2021
Michael Weedman

Age: 42
Location: AR
Admitted: 01/20/2022
To: Conway Regional Medical Center
Murdered: 01/24/2022
Perry James Ryan Traw

Age: 50
Location: ID
Admitted: 09/05/2021
To: St. Alphonsus
Laura L. Baker

Age: 78
Location: PA
Admitted: 08/17/2021
To: Jefferson Regional
Murdered: 08/31/2021
Nelson L Windsor

Age: 67
Location: IA
Admitted: 05/28/2021
To: St Lukes Hospital in Cedar Rapids, IA
Murdered: 06/27/2021
Ronald Pettit

Age: 31
Location: CA
Admitted: 11/05/2021
To: Kiaser
Donna Pena

Age: 72
Location: WA
Admitted: 01/01/2022
To: PeaceHealth Southwest hospital
Murdered: 01/24/2022
Wendy Gene Nickelson

Age: 43
Location: CA
Admitted: 07/16/2021
To: Natividad Medical Center
Narciso Serra

Age: 50
Location: MI
Admitted: 12/08/2021
To: Chelsea hospital/Allegiance
Murdered: 12/21/2021
Shawn Norman

Age: 64
Location: NY
Admitted: 12/08/2021
To: NY Presbyterian/Weill Cornell Medical Center
Murdered: 01/31/2022
James P. Traynor, Jr.

Age: 62
Location: TX
Admitted: 08/11/2021
To: Good Shepherd Hospital
Murdered: 08/26/2021
Larry Randall Wyatt
Age: 70
Location: FL
Admitted: 10/03/2021
To: Osceola Regional Medical Center, Kissimmee, Florida
Murdered: 11/02/2022
Kent F Schuch
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.