
Janet and Chris’s Story
Age: 61
Location: VA
Admitted: 08/13/2021
To: Centera Williamsburg
Chris Anderson


On January 26, 2022 my mom called me telling me she thought she was coming down with a chest cold and had made an appointment with her physician to make sure it wasn’t Covid and to get antibiotics. Wonder was a very active 73 year old woman living with COPD, and a week immune system. She had spent the previous weekend with me and my children to go watch the basketball games in to be with us because we had to put our dog down. She was very involved in my in my children’s lives. Although she was a high-risk candidate for complications if she were to have contracted COVID-19, her family physician out of liberty Missouri didn’t get her in for an appointment until Friday. At her appointment she was prescribed steroids and a Z pack and told to go home while they processed the lab results which didn’t come back to her until Sunday, January 30, 2022.
I remember receiving the text message from her that evening as the Chiefs were in the playoffs, telling me that her test results were positive for COVID-19 and not to come over the following day. She was fearful that she would pass on Covid to me. On January 31, Monday I went to her house to help take care of her and my stepfather, who had gone for a follow up visit with his physician from suffering with bacterial pneumonia. His physician did a rapid test so before he had reached home, we had received a phone call saying that he tested positive for COVID-19 as well. My mom is physician had referred her to liberty Hospital for monoclonal antibodies. Tuesday morning I contacted liberty Hospital to see when we would be scheduled for her monoclonal antibody injected, and was informed that they did not have any to give and would not know when More we’re coming as they are issued from the state. I called a nearby hospital to my mothers home, North Kansas City Hospital to see if they had any monoclonal antibodies and if she could be referred there quickly. I confirmed that they did have monoclonal antibodies and contacted her family Doctor Who sent the referral to North Kansas City hospital. We then were scheduled to go in the morning of February 3.
Unfortunately, on February 1 round 8 o’clock in the evening my mother’s oxygen levels dropped to 82 and I decided I needed to take her to the emergency room. Upon arriving I checked her in let the ER know that she was scheduled for monoclonal antibodies at that hospital and told them that I would bring her medications’ that she takes regularly down as well as asked that she receive vitamins B, C, zinc right away, due to the fact that she was immuno compromised. I was not allowed to go back with her so I gave her a hug as they wheeled her away. It wasn’t until February 5 that I was notified. She was given remdesivir beginning the evening of February 1st. Luckily, my mom had her cell phone so when a physician would come to visit, I had asked her to put me on speakerphone so that I could be involved in hearing what they were saying because we did not know she had received from the severe and we were not provided a list of medication’s, they were giving her. We both were very concerned that her oxygen need requirement was doubling daily. I contacted Dr. Molly James out of St. Louis after hearing about her from a friend of the family and hired them to provide proper medical treatment for my mother after being in the hospital for a week and isolation and not getting proper treatment, including not even being seen by a pulmonologist. The evening I tried to get her out of North Kansas City Hospital the nurse over seeing her room to told me she had to get the charge nurse when I told her I was there and we wanted to leave AMA due to lack of medical treatment and physician oversight.
The charge nurse told me that my mom was not well and it was a bad idea for us to leave. I stood there with a portable oxygen tank and explained our reasons for wanting to leave. I had my mom on the cell phone as she was down the hall in Covid. Isolation. She was on 10 to 14 L of oxygen at this point so she was unable to come off of their oxygen and walk to me. They refuse to take my oxygen tank to her or let us use one of the hospital wheelchairs I was then told if I tried to go to her room or use their wheelchair I would be escorted out by security if we waited until the morning when the doctors were back, we would be able to get a doctor to doctor transfer . What I found out the following morning is that the doctor on staff refused to give a doctor to doctor transfer for my mother. I went out and bought a wheelchair and was going up to the hospital when I received a call that she had taken a downturn and now was on over 30 L of oxygen, and moved to the cardiac wing, she now had become diabetic and was requiring insulin as well as having heart issues. They were also notations in her medical records stating potential acute renal failure. My mother had never had kidney problems prior to this nor was she taking insulin.
While she was in the hospital, I was told by the nursing staff that she had not been receiving her steroid inhalers properly around her fourth day, and that they had spent time with her to show her how to properly use those. She was refused vitamins for the first three days, and when I brought this up to the hospitalist, I was told that vitamins would not save her. I requested a list of the medication’s. I’ve been prescribed to treat my mother, those were medication, such as Pepcid AC, anti-inflammatories steroids, a cholesterol medication, montelukast, ivermectin to name a few. The hospitalist Dr. Vossler told me that montelukast was in trial studies, but could not be administered to my mother along with the others I was requesting because they were not CDC approved. Her opinion of ivermectin was that she does not give patients a warm medication when they don’t have worms, because she is not like one of those cowboy doctors that you’re hearing about on the news.
I again asked if the medication I was requesting would not cause her any harm potentially is the only reason because it is not CDC approved, and was told yes.
It wasn’t until her 20th day in the hospital that I was allowed to visit her. Visiting times were for limited hours and I had to be out of her room by 5 PM.
There were 2 different three hour slot times that I was allowed to visit throughout the day.
I spoke to every nurse on duty while my mom was in the hospital, it was never clear when the doctor would actually visit her and if I missed the call from the hospital from the doctor, or my mom forgot to put me on speakerphone, I would not be able to speak to a doctor on most days and would have to wait until the following day. The food service was set up where my mom would have to order the meal of her choice for breakfast, lunch and dinner if she did not pick up the phone and place her order she did not receive the meal. There were many times I took food down to her because she called to telling me how hungry she was and that she was unable to get any food.
I began sneaking in some of the medication‘s in a goodie bag that I would take down to her with food, books, Diet Coke, a dvd player with movies etc.
There were times where they would delay taking my mom, her goodie basket, and she would find that her food was cold by the time she received it however, if she ask them to warm it up for her, they would tell her know that they could not remove any of the items from her isolation because they might be contaminated.
I found out that respiratory therapy wasn’t working with her and physical therapy wasn’t either the notes on her record for an evening. Nurse said that she was resting when they would try to visit so they did not wake her. Respiratory therapy came in on one day that I was in her room. The respiratory therapist took down notes based on her monitors, and started to leave the room without even talking to my mom about how she was doing.. I stop the respiratory therapist and asked her about breathing exercises for my mother, proning, and massage techniques. I asked if these things could help and was told yes that she had a spirometer. I told the respiratory therapist that she wasn’t using the spirometer because it was too painful and asked if we used a cup with water in it, and a straw if that would be a form of exercise, that could be helpful and was told yes. She didn’t leave the room.
The last Thursday of February 2022 my mom’s oxygen needs worsened. When I came to visit There were multiple nurses in her room, and I was told that they had tried to put a BiPAP on her, but it was not administered appropriately and she was recovering from that. Within 10 minutes she was rushed to ICU where I took the elevator to meet her. They had a new staff member on the ICU floor that we were told administers BiPAP machines often and knew what he was doing. I told my mom that if there was anything uncomfortable I would make them stop and so she agreed once she was on the BiPAP machine. The air pressure was so uncomfortable. She started having hallucinations. I had to leave the room briefly, and when I returned, they had restrained her. I told them I did not want her on restraints, and I would sit next to the bed with her. It was been brought to my knowledge that something was wrong with her bed, and that they would have to have someone else in the room as well. Around 430. I had the choice to give permission of putting her on a ventilator and was told that it was necessary. I approved it and had to leave the hospital room at 5 o’clock Perll Hospital Rules due to the COVID-19.
Roughly 12 hours following her intubation, I was called and was told that her right lung collapsed. Every time I called the ICU to check in on my mother and spoke to the nurse. I was asked if I was ready to take her off of the ventilator and moved to comfort care.
When I arrived at the hospital on 26 February I told the staff I wasn’t going to leave until I met with the doctor. My mom had been there since February 1 and I had not met one doctor face-to-face I waited 3 1/2 hours and met with Dr. Lovett if edition, who had treated her on and off throughout her stay. We evaluated three days of x-rays of her chest. Because she had been put on multiple antibiotics, and I had been told that there was a possibility of her having bacterial pneumonia. I questioned that the x-rays I was being shown was certain positive Covid damage when I asked if it could be from bacterial pneumonia as well. The answer was possibly. Her vitals were fine and I had been told she had been put on palliative care without my permission. I demanded that that not be the case that I had never approved that and was her medical power of attorney.
On February 28, I received a call from the physician stating that my mother was unresponsive to some of the reflex tests they do. No gag reflex nor acknowledgement when they lowere sedation. That evening I approved her to be taken off of the ventilator. I had never received a call from social workers although I had complained to the patient advocacy department twice. My assumption with social workers and hospitals is that they are there to assist and inform families with difficult decisions, such as removing a loved one from a ventilator. I had no idea that a person comes off of a ventilator and struggles to breathe for an unknown period of time as it’s different for every person.
My beautiful mother took deep, hard breaths for 20 minutes after being taken off of ventilation. After a few trips in and out by the nursing staff, I was then notified that she had passed. I was given a paper to sign releasing the hospital of any liability of her personal items and drove to her house to tell my 8 & 9 year old boys along with my stepdad that she was gone. Following her passing, I requested her medical records from North Kansas City Hospital. The first records I received had about 90% of the records stating comments removed from nursing staff and physician staff. So I requested a second.
On the second medical records, it was missing the last five days. So I requested a third. The third request had the full medical records, which were about 2000 pages. I hired an outside physician who had worked in pulmonology for over 10 years that was referred to me from a lawyer. She evaluated the records and found multiple places of neglect. One of the most challenging things I’m dealing with now is finding a law firm to help me. My goal is that my mother’s death doesn’t become just another statistic. I lost my mother, my best friend, my children’s grandmother. Had the physicians and staff treated her with monoclonal antibodies vitamins, and other non-CDC approve medication’s my mother would be alive. This must be stopped for the future of our children and our freedom.
Filter By Category

Age: 61
Location: VA
Admitted: 08/13/2021
To: Centera Williamsburg
Chris Anderson

Age: 43
Location: AL
Admitted: 09/08/2021
To: UAB West
Murdered: 09/17/2021
Todd Abbott

Age: 60
Location: TX
Admitted: 09/05/2021
To: Decaunter and Jacksboro
Murdered: 09/08/2021
Walter Henry

Age: 66
Location: FL
Admitted: 07/15/2021
To: Palms West Hospital in Loxahatchee, Florida (Palm Beach County)
Murdered: 08/01/2021
Michael H. McVan

Age: 71
Location: MI
Admitted: 12/30/2021
To: Troy Beaumont
Murdered: 01/20/2022
Paul Korff

Age: 60
Location: OH
Admitted: 09/21/2021
To: Cleveland Clinic Main Campus
Murdered: 10/14/2021
Russell J. Kocka

Age: 69
Location: FL
Admitted: 08/14/2021
To: Advent Health Altamonte Springs
Murdered: 08/22/2021
Wayne Oliveira
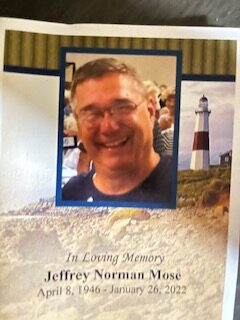
Age: 76
Location: MI
Admitted: 01/08/2022
To: Beaumont Hospital, Troy, MI
Murdered: 01/26/2022
Jeffrey Norman Mose

Age: 49
Location: NC
Admitted: 09/07/2021
To: Hugh Chatham Memorial Hospital and Atrium Health Wake Forest Baptist - Wilkes Medical Center
Murdered: 10/22/2021
Tim Rutherford

Age: 70
Location: MI
Admitted: 12/05/2021
To: Munson Healthcare Charlevoix Hospital (Michigan)
Murdered: 12/08/2021
Robert Michanowicz
Age: 77
Location: FL
Admitted: 07/09/2021
To: Jackson Hospital, Marianna FL
Floyd Hansbury

Age: 43
Location: WI
Admitted: 09/03/2021
To: Bellin Memorial Hospital, Green Bay, WI
Murdered: 10/10/2021
Doug Roatch

Age: 50
Location: KY
Admitted: 07/29/2021
To: Baptist Hospital
Murdered: 08/31/2021
Jason Fassler

Age: 53
Location: CO
Admitted: 01/15/2022
To: Rose Medical Center and Swedish
Jeff Nuttall
Age: 62
Location: FL
Admitted: 08/03/2021
To: St. Cloud Regional Medical Center
Murdered: 09/30/2021
Samuel E. Perez
Age: 72
Location: AR
Admitted: 11/26/2020
To: Yes
Murdered: 12/17/2020
Douglas A. Morriss

Age: 43
Location: AZ
Admitted: 11/04/2021
To: Mountain Vista Medical Center
Murdered: 11/20/2021
Karl Michael Esguerra

Age: 51
Location: MT
Admitted: 08/17/2021
To: At Vincent Healthcare and Advanced Care Hospital of Billings Montana
Dyan Wilson

Age: 74
Location: NJ
Admitted: 09/06/2021
To: Atlantic Health System, Morristown NJ
Murdered: 09/10/2021
Diane P. Bates

Age: 85
Location: AZ
Admitted: 01/17/2022
To: Yuma Regional Medical Centre
Murdered: 01/20/2022
Jeanette E. Chapman

Age: 71
Location: OK
To: Undisclosed
Murdered: 02/25/2022
Lloyd William Blansett

Age: 24
Location: NY
Admitted: 11/10/2021
To: Columbia Memorial Hospital and Westchester Medical Center
Murdered: 12/08/2021
Jeremy Budik

Age: 53
Location: NC
Admitted: 09/23/2021
To: FirstHealth Moore Regional Hospital
Doug Curry

Age: 73
Location: OH
Admitted: 12/29/2021
To: Clinton Memorial Hospital
Murdered: 01/17/2022
Connie Mae Moore
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.