
In memory of Anna Caruso victim of NIH/FDA protocol.
Age: 65
Location: NY
Became sick: 12/23/2021
First sought care: 01/08/2022
Admitted: 01/08/2022
To: Good Samaritan Hospital
Anna Caruso


My family went to Disney World on 1/27/22. My mother joined us on this trip. She fell ill on 1/30/22. She had a slight fever, around 99, but claimed to not be short of breath.
To give a little history, my mom was three years clear of lung cancer (limited to one lung, and received no chemo – just radiation), so my greatest concern with COVID-19 from day one with her, was it affecting her lungs? She never needed any oxygen and was in great shape otherwise. Lived alone, was out and about daily, drove, needed no assistance. Sharp as a tack.
She made it clear when COVID-19 first happened, “If I ever get covid, I don’t go to a hospital. Even if that means I die.” I agreed with her. We tried to treat her ourselves on the trip, including with ivermectin (although in hindsight, the dosage was not enough). By 2/6/22, she could barely muster the strength to walk far.
On the drive home, we stopped at a hospital in Kentucky. It was there that she was officially diagnosed with COVID-19. Her pulse ox was in the mid to high 80’s. They suggested she stay the night, especially since it was possible she could have had a NSTEMI heart attack (days later, that didn’t appear to be the case, per St. Joe’s). She refused, and we drove home.
At my home in White Lake, MI, my friend who is a PA, examined her. The plan was to order her monoclonal antibodies the next day. Another friend loaned me her oxygen (the backpack type that takes in air from the outside). We got her pulse ox up to the low 90’s. My mother had a few bites of spaghetti, and then napped.
I checked her pulse ox when she woke up, and it was in the 80’s….it started to desat to the low 70’s and then 69. This frightened me, and I called an ambulance. My mother understood, but was angry at the same time. She said, “I don’t want to be intubated, and I don’t want remdesivir.” I reassured her that “I will make sure that doesn’t happen.” When I called 911, I explained to the operator (I’m sure there is a recording out there somewhere of this conversation) that my mother doesn’t want either of those two actions. She wanted to go to University of Michigan (U of M), because they have better visiting hours and better staff. The EMT’s refused because of the distance and we were stuck with St. Joe’s. I followed the ambulance and walked into ER to reiterate my mother’s wishes.
That night, I talked to her while she was in the ER. She said, “Come pick me up..they are talking to me. I don’t trust them.” I called the nurse’s station, and also talked to the doctor. “Please stop talking remdesivir to her. She doesn’t want it. She wants me to check her out. I can’t care for her here. She needs to trust you.” They agreed, and said “She’s the boss. We will let it go.”
The next a.m., she is in her own room now. I talked to her and she told me, “The nurse came in this a.m., and was reading off the meds, and brought up remdesivir as being on the list. Diana, I don’t trust them. Get me out of here. I wouldn’t be surprised if they slip it in.” Angrily, I call them, and they apologized, claiming, “Sometimes the messages from the ER don’t get to us in time.” That is a scary thought. I told them, “Make it clear to them to stop, because she has checked herself out before. She will do it again. I don’t care if you need to put a sign on her door, spread the message and make it stick!” That is what they did. The nurse put a sign on her door, reading, “Please do not mention the medication remdesivir to the patient.” There was also a small stick note by the sink where the provider washes, stating the room number and “no remdesivir.” There are photos of these signs.
When I went to visit her, she had a nasal cannula and looked great. She was walking around, talking on speaker phone, etc., to my sister …she was laughing….I think having the iv fluids helped because she hadn’t eaten or drank much prior. It was a great evening, and I went home after visiting hours.
The next day, after dropping off my kids at school, I received a phone call from my mom, screaming, “Get over here now, please, and hurry! They are beating me up!” I drove so fast, and texted her when coming up the elevator I was almost there. She now had a non-rebreather on her and she was very upset. They claimed she got up to go to the bathroom and started to desat. So they forced this non rebreather on her. Apparently they were rough handling her. I gave them the benefit of the doubt that she may have needed that and was fighting them on that. I don’t know because I wasn’t there.
That night when she needed to be moved up, two male nurses/attendees (not sure position) started to lower her bed and move her without explanation like a rag doll. She started to ask, “What are you doing…stop…stop…STOP!” I’ve never seen my mom almost cry out of terror, and it caused me to scream, “STOP!! STOP! She asked you to stop – you stop!!” His response was, “Well, she wasn’t listening to me.” My mother and I in unison, replied, “No, YOU weren’t listening.” I asked them to leave and called the Chief of Staff, Fabian Fragoli’s office, and complained. I also requested they not be allowed back in the room. One of those men apologized on their own.
With the non-rebreather attached, it was difficult to understand her, so at that point I brought her a notebook and pen. I still have this. She wrote, “Please don’t leave me, they are not as nice when you leave.” Something to that nature…I have a photo of this. At that, I found a way that I could stay at the hospital 24/7 if I sign on as a caregiver.
The first day or two in the hospital, an individual did call me to talk about a plan for when she was released. That was the only conversation about that. They asked her if she would ever want a ventilator. She said, ” No.” Doctors did ask my mom, “If your heart were to stop, do you want chest compressions? ” She said, “Yes, of course.” Then they proceeded to tell her, “Because of your age, if we did chest compressions, we’d probably break/crack your chest and ribs, and then would have to ventilate you. Did you want that?” She disappointedly said, “Well, then, no, I guess.” She made it clear she wanted all measures taken to save her. She just didn’t want ventilation. I asked them to stop having this same conversation with her. It was so negative, as if they expected her to die, and she looked/seemed well to me!
It was 2/8 or 2/9 (I have to look in my notes, for an exact date), I was on speaker with my cousin, who happens to be an oncologist/hematologist, and Dr. Shamla Kalyan (infectious disease doc) walked into my mother’s room and says, “I know, I know, you don’t want me to mention remdesivir, but I tell you, it kills the covid.” My cousin, hearing this, scoffs, “It doesn’t kill covid and you know it. It is supposed to stop the replication, but there is no proof that it does that.” Dr. Kalyan proceeded to agree that if her blood work goes sideways she would back off the remdesivir. She also agreed to give her an antibiotic (she had previously refused our request for one because the covid being viral in nature) if she started on the remdesivir.
The night my mom started on remdesivir, she had a dark bowel movement. There was a trace of blood in her stool and so they backed off the lovenox. They also suggested a bipap because she coded that evening after getting up to use the bathroom. My mom didn’t want the bipap, but the nurse and I got her to agree under the conditions; it was only for the evening, and if after that, she wanted it off, at any time, she could have it off. It is also important to note that from the day she was admitted, the doctor recommended an x-ray every day. At one point her lungs were improving.
Over the next couple days, she hadn’t had any food because of the bipap. No one ever did remove it for her. She did have fluids I believe, intravenously, but no food. When no one brought it up, I did. Finally, they agreed to give her a tpn (total parenteral nutrition). They also got her a DNR bracelet after asking again if she wanted intubation. In their notes, they mention talking to me about the DNR, and me understanding. No one talked to me about the DNR. No one. Besides, DNR does not mean, do not treat.
I asked about the antibiotic Kalyan promised. No one could answer that. They claimed she said, “No”…even though she promised us.
We would see Dr. Lejoie and the other rounders from Clarkston Medical Group. They would pop in for a few minutes and be out again daily.
My mom was able to practice twice being off the bipap. The first time was 20 minutes before she started to slowly desat. This was after being on the bipap for a day or two. She wanted to practice more often, but there is only one respiratory therapist for 3 floors, including ICU. So, they were scarce to appear. When they did, they were in and out. The female one would refuse attempts off the bipap to practice independent step down breathing. Finally a day or two before my mom’s passing, she did allow it, and my mom lasted and held her saturation for 45 minutes. She could have done longer, but because it was difficult to get a hold of the respiratory therapist, she asked me to bring her back early just in case she wasn’t around if we needed her. My mom was about to stay around 95/96.
The every other day x-rays just randomly stopped on the 11th or th12th of February. I don’t know why. The lovenox, I believe, was finally reintroduced but it was more therapeutic…not full dose.
On February 15th, my mom’s pulse ox was 95-98. Then I noticed it start to slowly dwindle. It made no sense why. I started to page nurses that didn’t answer my calls or were nonchalant, kinda like, “I don’t know…we will let the doctor know.” I figured they were just busy, and even though they weren’t responding like I’d like, I didn’t really blame them, as why they were short handed. Looking back, I feel like everyone was letting her die….or knew she was dying…except for me…and they wouldn’t tell me that either. I was told early on, that despite visitor rules, they will allow immediate family to come to say their goodbye’s if a patient were in dire circumstances.
For 8 hours or more, I tried to get a hold of Clarkston Medical Group where Dr. Lejoie was out of. There was no emergency number for him, and all I’d get is annoying jazz hold music. So between paging the nurses and waiting a half to a full hour for someone to help her, whether it be changing bed pan, position, or find out where the doctor was, I was in panic. I watched her pulse ox go from 98 to eventual death. No x-ray ….and I asked many times about it to the point that I texted my own doctor, out of the same practice, to help me get her help. I have screenshots of all those texts and cell phone bills …call button timers to show this. My mother even wrote in her last few hours in that notebook, “This is barbaric.” “I’m not going to make it.” “Afraid” “Escape.”
The concierge refused my sister to come up to say goodbye to our mom. She told her, “To my knowledge, Phyllis isn’t dying. Till the doctor tells me she is dying, she’s not dying.” Then she came up to me while I was on speaker with my cousin on the phone who is again, a witness and a doctor himself, and she said to me, “Are we treating Phyllis, or giving her comfort care?” I didn’t understand what she was asking me, but my doctor cousin said, “I hope you’re treating Phyllis aggressively.” She said, “Ok then, and walked away.” I didn’t see her again untll she came into the room and yelled at me for not having my mask on while I was saying goodbye to my mom. I do have audio recording of that scolding during that emotional moment. She tried to get me to leave, but I refused.
My mom died shortly after. I was able to call each sister while they said goodbye over the phone to her ear. I asked for heparin, we got none. I asked for an antibiotic, but we were refused. The same antibiotic we were promised if she took remdesivir. They let her circle the drain and do nothing to clinically assess why the turn for the worse. They would take her blood, and give her a sedative, but not an x-ray or any other tests.
She died around 10:20 a.m., or that’s when they called it. I think it was closer to 10 a.m. A few minutes prior, Dr. Lejoie prances in and I yelled at him, asking him, “Where they hell have you been?” He was offended that I questioned his tardy attendance, leaned over and whispered in a condescending tone, “I think your mom had a micro embolism. Would you like her to have comfort care?” I turned to her and then to him, “I think she is already dead, but in case she isn’t dead enough, sure.” I didn’t know what to say…she looked dead. She suffered so greatly before. It was like watching someone suffocate….couldn’t tell if she had passed or passed out. Needless to say, she never received comfort care, and I yelled at the doctor. Then Dr. Kalyan came in and just stared at me and my mom till I kicked her out. I looked up at the white board in my mom’s room…you know, the one that gets updated daily. It was still dated 2/14…my mom died on 2/16. Needless to say, that must have been the time they stopped treating her.
I met with Dr. Fragoli, Chief of Staff or similar title for St. Joes (Trinity Health) in Pontiac. Show him and his secretary nearly all the complaints I had. At that time, I wasn’t looking to sue, I told them I wanted answers, action, and corrections. I will include the letter of response from him after the meeting, as well as my response to his response. While I have proof that Dr. Kalyan agreed and bribed my mom to take the remdesivir, but she denied it to him. I have proof of everything I am saying as to feel comfortable naming names and making claims. I did file a complaint with the state licensing board, and included all, but I just got the standard, “we cannot find any wrong doing response.” I was warned that they’d get away with it, but it was good to file the complaint regardless.
Filter By Category

Age: 65
Location: NY
Became sick: 12/23/2021
First sought care: 01/08/2022
Admitted: 01/08/2022
To: Good Samaritan Hospital
Anna Caruso

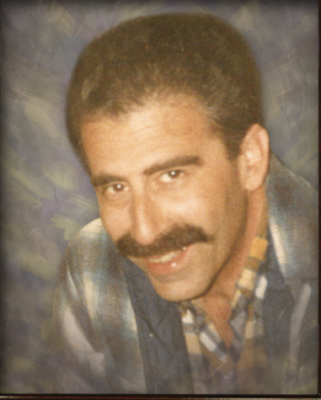
Age: 53
Location: OH
Became sick: 12/25/2021
First sought care: 01/04/2022
Admitted: 01/04/2022
To: Clinton Memorial
Murdered: 01/29/2022
Todd L. Pointer

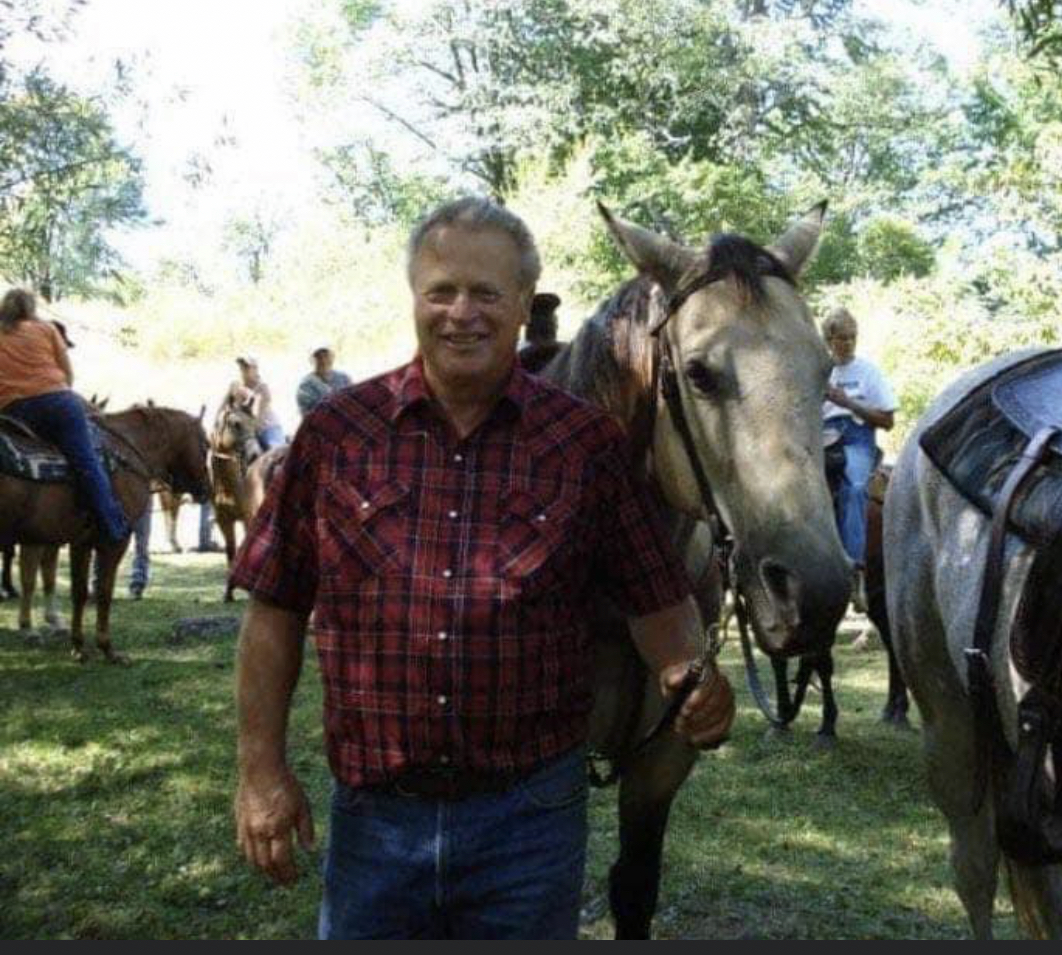
Age: 61
Location: VA
Became sick: 08/10/2021
First sought care: 08/13/2021
Admitted: 08/13/2021
To: Centera Williamsburg
Chris Anderson

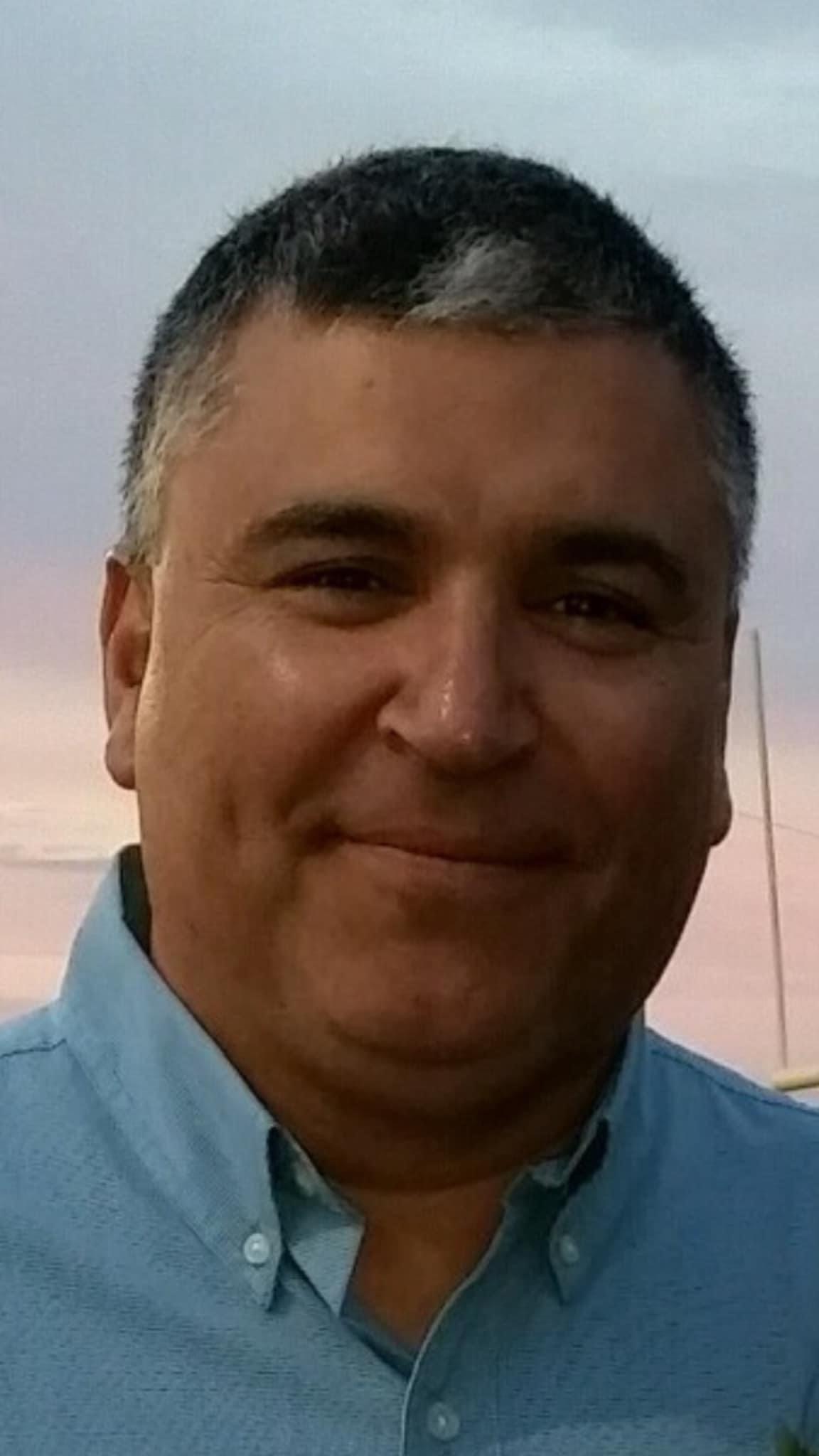
Age: 80
Location: OK
Became sick: 09/20/2021
First sought care: 09/23/2021
Admitted: 09/23/2021
To: St Johns and Hill Crest
Murdered: 09/29/2021
Ron and Pat Mills

Age: 62
Location: CA
Became sick: 12/23/2021
Admitted: 12/27/2021
To: Los Robles Hospital
Murdered: 01/09/2022
Abilio Ramos and Dawn Michael

Age: 43
Location: AL
Became sick: 08/31/2021
First sought care: 08/31/2021
Admitted: 09/02/2021
To: Northside guntersville al
Murdered: 09/23/2021
Shannon Marie Jordan McDonald
Age: 79
Location: AZ
Became sick: 01/04/2022
First sought care: 01/06/2022
Admitted: 01/06/2022
To: Honor Health Deer Valley
Murdered: 01/16/2022
Charles F. Shepherd
Age: 78
Location: WI
Became sick: 09/21/2021
First sought care: 09/26/2021
Admitted: 09/26/2021
To: Bellin Hospital Green Bay Wisconsin
Murdered: 11/06/2021
Lawrence (LJ) Sperberg

Age: 70
Location: TX
Became sick: 08/19/2021
First sought care: 08/19/2021
Admitted: 08/19/2021
To: Texas Health Harris Methodist Hospital
Murdered: 09/01/2021
Tennis Ingebretson

Age: 66
Location: TX
Became sick: 09/17/2021
First sought care: 09/26/2021
Admitted: 09/26/2021
To: CHRISTUS Trinity Mother Frances Hospital
Murdered: 11/17/2021
Sylvia Rodriguez

Age: 71
Location: NY
Became sick: 08/21/2021
First sought care: 08/24/2021
Admitted: 08/24/2021
To: Good Samaritan
Murdered: 10/06/2021
Anne Wishniak

Age: 64
Location: TN
Became sick: 09/09/2021
First sought care: 09/10/2021
Admitted: 09/16/2021
To: Cookeville Regional Medical Center
Murdered: 10/10/2021
Steven Gilbert Martin, Sr.

Age: 59
Location: NJ
Became sick: 05/02/2020
First sought care: 05/02/2020
Admitted: 05/02/2020
To: Community Medical Center and Arista care
Murdered: 06/02/2020
Linda Pichirallo

Age: 71
Location: MI
Became sick: 12/21/2021
First sought care: 12/23/2021
Admitted: 12/30/2021
To: Troy Beaumont
Murdered: 01/20/2022
Paul Korff

Age: 71
Location: TX
Became sick: 11/15/2020
First sought care: 11/24/2020
Admitted: 11/24/2020
To: University of Texas Medical Branch League City Campus
Murdered: 12/17/2020
Gene Craig Chaudoin
Age: 51
Location: TX
Became sick: 07/20/2021
First sought care: 07/21/2021
Admitted: 07/24/2021
To: 1. Shoreline in Corpus Christi, 2. Doctors Regional Corpus Christi
Murdered: 08/25/2021
Edward M. Garza

Age: 65
Location: MN
Became sick: 12/23/2021
First sought care: 12/29/2021
Admitted: 12/29/2021
To: Allina Health in Faribault, MN and transferred to Abott Northwestern in Minneapolis, MN.
Murdered: 01/10/2022
Paul Jerome Swenson

Age: 54
Location: OH
Became sick: 08/25/2021
First sought care: 08/27/2021
Admitted: 08/29/2021
To: Wooster Community Hospital
Murdered: 09/16/2021
Angela Plant

Age: 71
Location: MI
Became sick: 11/24/2021
First sought care: 11/24/2021
Admitted: 11/24/2021
To: McLaren Hospital, Mount Clemens
Murdered: 01/02/2022
Charles V. Domine; aka Chuck

Age: 56
Location: TX
Became sick: 12/22/2020
First sought care: 12/25/2020
Admitted: 12/25/2020
To: Baylor Scott and White All Saints Medical Center
Murdered: 02/03/2021
Ed Hodges

Age: 51
Location: NY
Became sick: 01/18/2022
First sought care: 01/25/2022
Admitted: 01/25/2022
To: St. John’s Episcopal
Murdered: 02/13/2022
Jamell Jones

Age: 77
Location: MA
Became sick: 09/19/2021
First sought care: 09/23/2021
Admitted: 09/23/2021
To: Melrose/Wakefield Hospital
Murdered: 10/01/2021
Frank C. Bourgeois

Age: 56
Location: WY
Became sick: 09/30/2021
First sought care: 10/07/2021
Admitted: 10/16/2021
To: Wyoming Medical Center
Murdered: 11/03/2021
Richard “Zak” Szekely

Age: 50
Location: SC
Became sick: 09/02/2021
First sought care: 09/10/2021
Admitted: 09/10/2021
To: Roper St Francis Mt Pleasant Hospital
Murdered: 10/13/2021
James V. Lamb, III
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.