Euthanized by Kaiser Hospital
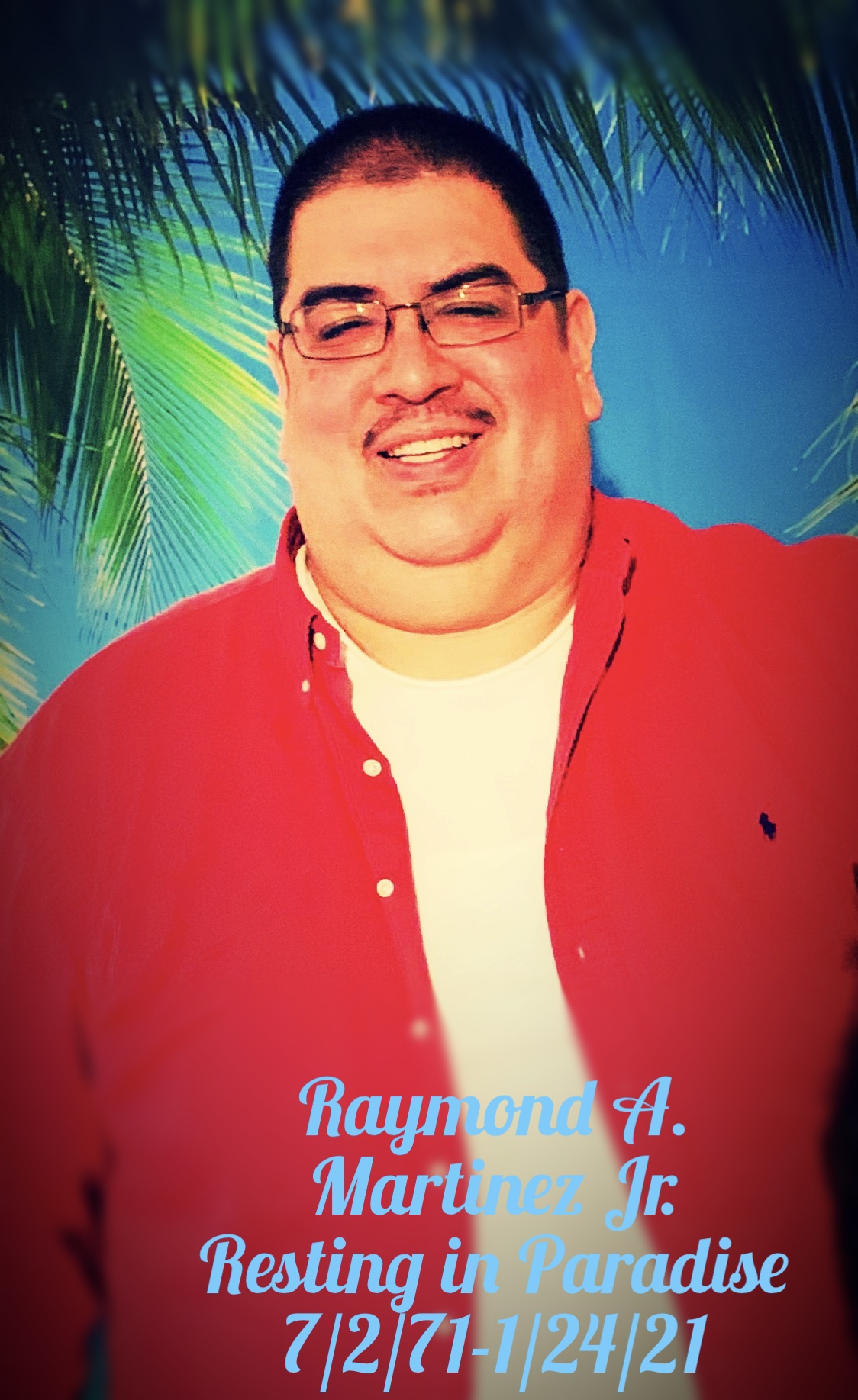
Age: 49
Location: CA
Admitted: 01/24/2021
To: Kaiser
Murdered: 01/25/2021
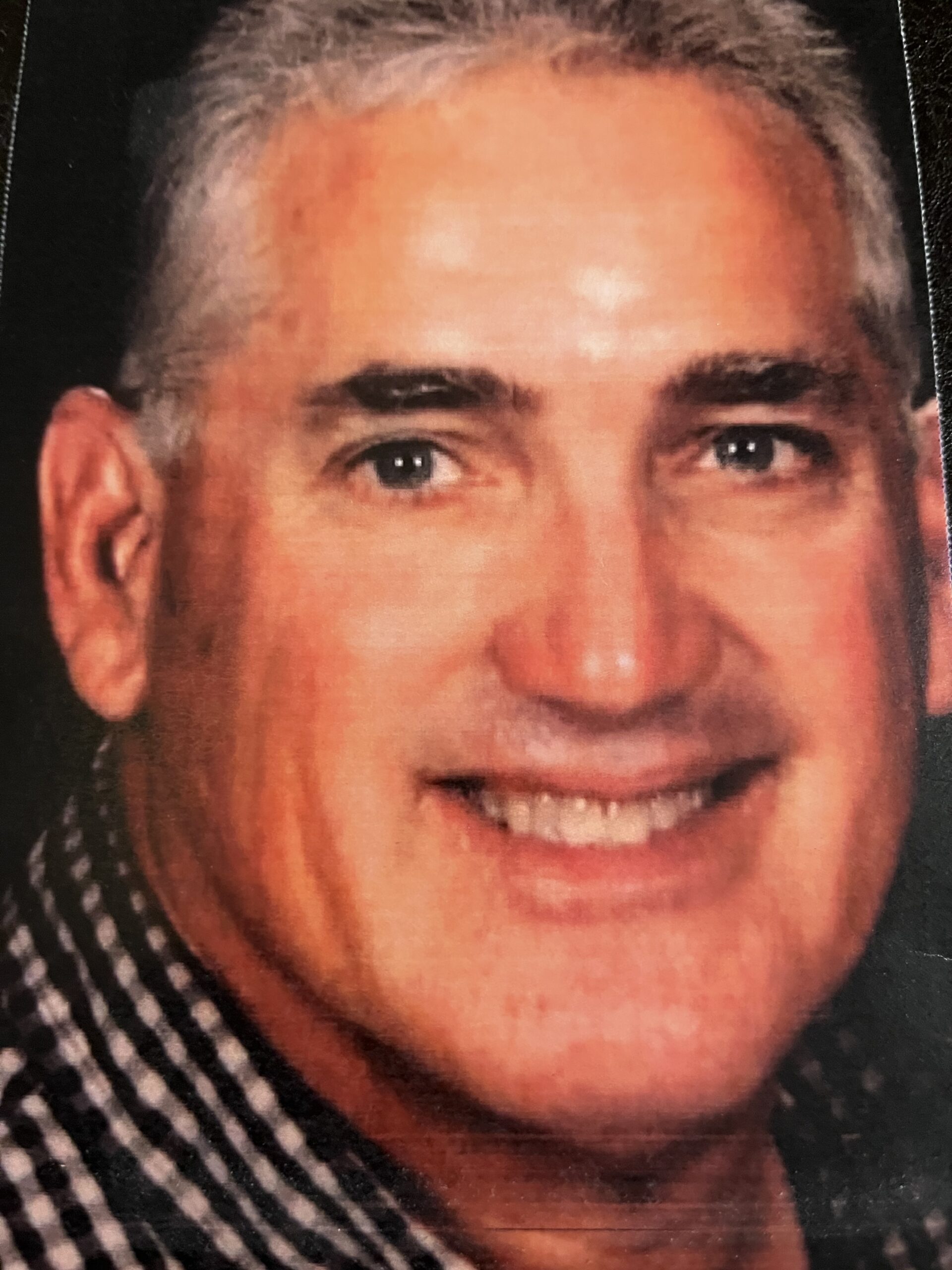
Raymond Albert Martinez


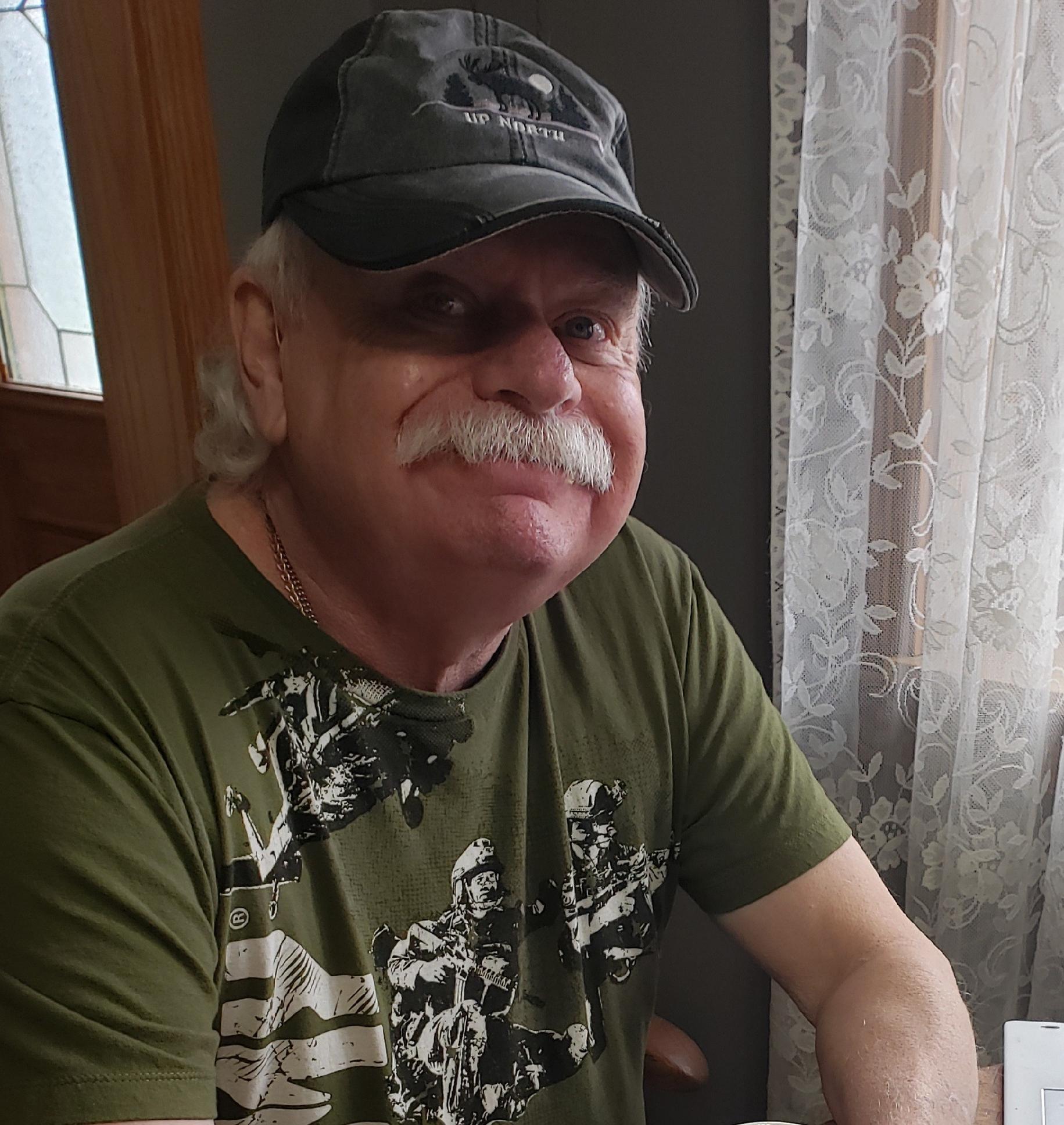
Shannon checked all the boxes - 65 year old male, diabetic, "refused" the vaccine, complained about his oxygen, wasn't allowed to question his treatment plan, tried to participate in his own care, staff ignored him and dismissed his concerns. He felt he was suffocating from the high levels of oxygen being forced upon him. Nursing refused to address his discomfort and he was considered non-compliant. . Nursing refused hydration and nutrition. He was terrorized, gaslighted and bullied, and treated like he deserved to be sick because he wouldn't obey and follow "the rules."
Thank you for the opportunity to share the story of Shannon’s unnecessary demise provoked by the Covid-19 Death Protocol. Shannon and I began our journey together in Wyoming in 1978, raising two wonderful men through many memorable adventures in several western states. Shannon had a rocky start in life; he was born prematurely, and his mom died when he was young. His father was unable to care for him properly, so he was taken in by his older siblings with young families of their own. All credit goes to them for the kind, decent, hard-working man he became. He was my life partner and best friend, a warm, loving supportive dad, an adored grandfather of three, a beloved uncle and a cherished friend to many. Family was everything to Shannon and he was certainly the hub in our wheel of life. The many people he loved and who loved him dearly still struggle to navigate the enormous, jagged hell left in his absence.
I had been sick for several days with pneumonia-like symptoms and was given a pulse oximeter by the Kadlec Urgent Care doctor. I was instructed to check my O2 regularly and go directly to the hospital if my sats fell below 90%. The Kadlec UC Doctor also asked why I had not been vaccinated for Covid and I told him our GP had retired and we were having difficulty finding a new one. He gave me a printout of options thru Kadlec, warning me the waiting time for an appointment could be five or six months. I called the Kadlec Residency Clinic when I got home to book appointments for both of us, but the earliest available were months away – September 28th and October 1st.
That afternoon, while demonstrating the pulse oximeter on Shannon, I noticed his O2 sats were fluctuating below 90%. Shannon had had a mild cough since the fire season had kicked up in July and it was starting to wear him down. Based on information from the UC Doctor, and out of an abundance of caution, our boys took Shannon to the Kadlec Emergency Department. After spending several hours in the ED Waiting Room, Shannon was admitted to the ED exam room for several more hours and finally admitted to the Acute Care floor at Kadlec Regional Medical Center in Richland, Washington the evening of August 11th, 2021.
The following morning, Dr. Kale called to update me on Shannon’s condition, stating Shannon “has bacterial pneumonia, but it looks like we’ve caught it in time, and he should be fine.” Shannon spent the next 10 days isolated in Kadlec Acute Care, assigned to Dr. Abir S. Abdel-Kader. Kadlec separated Shannon from his family except for personal cellphone calls for the remainder of his first hospital admission and family was forced to initiate all contact with Kadlec regarding his care.
Shannon frequently complained about feeling smothered by the elevated levels of oxygen being forced on him, but staff routinely ignored his questions and concerns. He was also frustrated about not being given adequate opportunity to discuss his condition with a doctor and the staff denied knowing what was going on. Our daughter-in-law is an RN, and with Shannon’s consent, she called the Nurse’s Station to check his status on the sixth day of his stay.
She was told he had just finished his fifth dose of Remdesivir, an off-label drug granted emergency use authorization by the FDA for the treatment of Covid. We were surprised as Kadlec failed to notify our family Remdesivir had been prescribed. Upon review of Shannon’s medical records, there was no documentation that Kadlec medical staff informed him about the drug, including its emergency use authorization or the potential side effects, and no evidence he signed any Informed Consent document.
Kadlec discharged Shannon home on August 22nd with an order for 10L oxygen, very vague follow-up instructions, and prescriptions for an oral steroid, over-the-counter cough medicine and an antibiotic. As was consistent with our experience, Kadlec neglected to reach out to his family to include us in his aftercare. Shannon continued to have low energy and poor appetite but was seeming to improve. He began to wean himself off oxygen as he said he’d been instructed and had managed to decrease his level to about 3L.
In the early evening, on August 31st, Shannon was trying to finish his schoolwork. He had returned to college for his Project Management Certification through an L&I Retraining Program and was in the process of taking the finals for his seventh quarter. He was due to graduate in December of 2021. Shannon was dedicated to his program and was an excellent student. I was reading his textbook aloud to him as he rested on the couch when he began to loudly wheeze and was struggling to breathe. We decided to call an ambulance as we felt it was the quickest way to get him the medical attention he needed. The ambulance responded immediately, set him up on a breathing treatment with oxygen and transported him to Kadlec.
Once at Kadlec, Shannon remained in the Kadlec ED exam room for almost 24 hours. Shortly after admission to the ED, Shannon called our younger son and daughter-in-law, stating that an unidentified doctor had told him he was “a dead man walking,” and that he would “likely be placed on a ventilator.” He was frantically asking our daughter-in-law what he should do, what he should ask for, what his treatment options were at this point. Shannon told them the doctors refused to prescribe a steroid because they said it was too late. Shannon’s medical records stated he was denied the steroid due to the risk of heart attack or stroke. His medical records also note that Kadlec administered Shannon a second Covid test that came back negative for the virus.
Shannon was a diabetic. He had routine visits with his diabetic doctor and was diligent about managing his diabetes, closely monitoring his blood sugar levels and making serious effort with his food intake and diabetic medications. Kadlec was aware of Shannon’s diabetes but neglected to provide him any form of nutrition until the mid-morning of September 1st, well over 15 hours after he’d arrived at Kadlec. He was admitted to the 9th Floor ICU Overflow Unit later that evening, requesting his blood sugar be checked and his diabetes medication given so he could eat dinner.
Out of desperation, he called complaining the nurses kept telling him they would order food shortly, but his meal never came, and he didn’t know what to do. He was upset and felt like he needed to eat something, but nursing ignored his concerns and refused to provide his diabetic medicine. I mentioned I had packed his diabetic supplies in his bag, and while we were still on the phone, Security suddenly stormed his room, searched his bag, and confiscated his diabetic medicine. Even at that point, staff failed to address his concerns and were evasive about providing his diabetes medication and refused him the nutrition his body needed.
When we talked again by phone, Shannon said the Kadlec doctors were waffling around whether to place him on a ventilator and he felt he was in a holding pattern. When I tried to express my reservations about Kadlec placing him on a ventilator, he became frustrated and shouted, “I may not have a choice, Diana!” Staff then entered his room, and he hung up. A few minutes later, he called back and said the doctor had decided it was not yet the right time to intubate and he was again suspended in limbo. Shannon’s intense reaction to my concern was disturbing and very uncharacteristic of him, and it was a red flag for me. Kadlec had successfully kept us apart and unable to fully communicate, and I felt helpless and unsure of what to do.
We contacted Shannon’s nurse at that point to inquire what was going on. During this conversation, I told Jessica, RN, that Shannon had not been himself for the last few weeks, confused and struggling, and asked her to please note in his chart to call myself, or one of our sons with all questions, information, or updates. I gave her our three cellphone numbers, and Jessica documented the information in his medical records. She stated that if the doctor did decide to intubate, he would call either before the procedure or directly after, but we would be notified.
Shannon was hypoxic, scared, and vulnerable in his confusion, and despite the family/POA’s requests to be contacted with all issues and updates, Kadlec neglected to include his family in all of the complex, life-threatening decisions they forced on him. Upon review of Shannon’s medical records, there was no signed Informed Consent document authorizing the ventilator or stating he understood the risks of the procedure, or the potentially deadly sedating, paralytic and opioid drugs that were administered to him.
At approximately 1:30 a.m., September 2nd, 2021, Shannon called my cellphone, but I was not able to pick up in time. He then called our older son and told him Kadlec had decided to put him on the ventilator; the doctors were on their way, and he was calling to let us know that he loved us. The doctors entered his room at that point and Shannon hurriedly said, “I got to go, I love you, good-bye,” and hung up. We waited for a call that never came.
First thing that morning, we called the nurse’s station to talk to Jessica, RN. She stated Shannon was stable and had verbally consented to being placed on the ventilator only if Kadlec would agree that if it looked like he was not going to make it, they would bring him back to say goodbye to his family. Kadlec agreed to Shannon’s last wish knowing full well that they would not be able to keep that promise. It was around this time, our older son arrived at our house and stated he had received a call from Ryan, a social worker from Kadlec, however he was unable to answer his phone at the time because he was driving. The voice message Ryan left stated he wanted to talk to us regarding “your father’s release.”
Later that morning, at 9:51 a.m., Ryan, SW, called my phone and after identifying himself, his first question was, “Can you think of anything that Kadlec may have done to contribute to the decline of your husband’s condition?” I thought this was a very peculiar way to begin the conversation and said, “Yes! I think you could have treated him for the pneumonia you said he had instead of the Covid he didn’t have.” Ryan had no response to that other than to ask if I was available to meet with Dr. Dany Ghannam at Kadlec Regional Medical Center at 1:00 p.m. to discuss Shannon’s care. Since I was still recovering from my own illness, I asked our older son if he was available to take me to Kadlec. At that point, Ryan’s voice sounded panicked, stating only one person would be allowed to attend and asked if I had been vaccinated. I confirmed I had not had the vaccine. Ryan then asked if we would be okay with a telephone conference instead, at the 1:00 p.m. time and I agreed.
At 1:00 p.m. on September 2nd, Megan, a second Social Worker from Kadlec, called to ask if I was planning to meet with Dr. Ghannam at the set hour and was unaware that we had arranged to talk via the telephone. At 1:16 p.m. Kadlec called back. Dr. Dany Ghannam was present along with Megan, SW and Colleen, RN, Palliative Care, Cathy, Case Manager and Jennifer, Shannon’s bedside RN. At this point, we were under the impression we would be meeting one-on-one with Dr. Ghannam only, and we were a little caught off guard there were other staff on the call. Both our sons were with me, and our daughter-in-law was participating via her phone. We asked how soon we could see Shannon and were informed about Kadlec’s limited visitation policy.
When asked what Dr. Ghannam’s estimate for length of time Shannon would be on the ventilator, he stated average time a patient usually spends on a ventilator is 2-3 weeks but did not think Shannon’s body would tolerate that long due to his heart being at risk. We asked what other interventions were being considered and if any additional tests were being ordered, but Dr. Ghannam failed to specifically address our questions. We were told Shannon would remain on a paralytic drug in prone position for 18 hours following intubation, and if he tolerated it well, he would be moved to supine, and the paralytic would be discontinued.
Dr. Ghannam also stated secondary infections had been ruled out, and expressed concerns that Shannon was not going to survive due to excessive scarring in his lungs, but he would continue to monitor him daily. Less than 10 hours after Shannon was placed on the ventilator, Dr. Ghannam was persistent our family transition him to Comfort Measures. The call ended at that point with the understanding that I could go to the hospital to see Shannon that day.
In the early afternoon of September 2nd, I arrived at Kadlec Regional Medical Center to spend the day with Shannon. When I got to his room, the door and curtains were wide open, all the lights were on and several staff were blocking the doorway, gawking, and whispering. I was emotionally gut punched to find Shannon stark naked, positioned on his stomach, his head turned towards the door, and only a small paper towel protecting his dignity. His Bedside RN, Jennifer, was standing at the far side of his room and appeared to be staring out the window. When Shannon heard my voice, he jerked his head towards me, his eyes flew open, looking around for me, his right arm shot out towards me, and he attempted to speak.
I rubbed his back to soothe him and explained he wouldn’t be able to talk due to the vent but if he could understand me, he could lift his eyebrows. He indicated yes by moving his eyebrows up and down. When I told him I loved him, he flinched his eyes several times and appeared to be crying. I asked if he was fighting to come back to us and he flinched his eyes several more times. I was stroking his back and arms and he began flopping in his bed like a fish out of water as if he were reaching for me to pull me closer. I asked him if he wanted me to call his sister and he indicated yes again. I called her and held the phone to his ear so she could pray over him and tell him she loved him.
After the call, I asked Shannon if he wanted me to rub lotion on his feet to make him feel better and he indicated yes. I rubbed the lotion into his feet and then covered them with socks, continually soothing him. I asked Jennifer if it was normal for vent patients to have that reaction, as it was obvious that he recognized me. Jennifer stated it would be very unusual as Shannon was paralyzed and unable to open his eyes or move, stating it was “probably my imagination,” then she adjusted one of his IVs and Shannon became unresponsive. I remained at Shannon’s bedside, comforting him, until visiting hours were over at 8 p.m.
During my visit with Shannon, I asked Jennifer about his condition and what was being done for him. I asked when he had last been fed and Jennifer denied knowing and stated Dietary would be assessing his nutritional needs and following up. She assured me he was being well taken care of and she would make sure I could get as close as possible during our visit. I stated that Dr. Ghannam had told us Shannon would remain prone and on paralytics for 18 hours following intubation, which I estimated to be about 8 p.m. that day, about the time visiting hours ended.
At that time, the paralytics would be discontinued if he was tolerating the supine position, otherwise he would remain prone until there was another opportunity to try supination again. Jennifer stated the process of moving a patient from prone to supine was complicated and took some planning and the involvement of at least four nursing staff members to execute as it had to be done carefully and slowly, so as not to cause further damage to the patient. She stated it was more likely to happen around 2 a.m. to ensure adequate staffing and time were available to do it properly.
I said good night to Shannon and left his room at 8 p.m. when visiting hours ended. According to Shannon’s medical records, he was repositioned from prone to supine at 2000 hrs. (8:00 p.m.) as I was leaving Kadlec for the day, which leaves me wondering what level of care and planning went into making sure Kadlec staff performed the transfer properly, safely, and humanely.
The whole situation felt off to me so when I got home, I reviewed Shannon’s MyChart and decided to print out his chart notes. I continued printing the chart notes when I got up the morning of September 3rd. I was preparing to return to Kadlec again when Shannon’s Bedside RN, Joshua called about 11:30 a.m. to tell us Shannon’s O2 was dropping and there was nothing else they could do. We rushed to Kadlec and up to Shannon’s room. Due to the decline in Shannon’s condition, the three of us were allowed to go into Shannon’s room despite the strict Visitor Policy.
As our sons and I gathered around him, Shannon regained consciousness and indicated he knew we were there, using his eyebrows and facial expressions to communicate. At one point, Shannon weakly attempted to reach towards his face, as if he were trying to pull on the ventilator. We asked him again if he was still fighting and wanted to come home to us and he indicated yes. We interacted with him for another 5 minutes or so until Joshua adjusted his IV meds and he slipped away.
At this point, Joshua told us Dr. Ghannam wanted to meet with us and led us to the conference room where the same Care Team from the previous day was assembled. Dr. Ghannam joined us a few minutes later and began rambling on about Kadlec’s pride in their communication skills when our older son interrupted him to confront him about that point, asking why the doctor hadn’t called when his dad was being put on the ventilator?
Dr. Ghannam seemed very confused about this, asking, “Nobody called you?” and our son reiterated that we had been told by Nurse Jessica the evening before Shannon’s intubation, that the doctor performing the procedure would call either before or immediately after and the reality was that Shannon called just minutes before to say goodbye and tell us that he loved us. Dr. Ghannam expressed surprise and frustration at this fact but failed to apologize or offer an explanation.
Dr. Ghannam also stated he was unaware that Shannon’s medical chart contained the results of test done during his first admittance, which indicated Shannon had suffered a mild heart attack sometime the three months prior. I asked if Shannon was at an increased risk of heart-related complications and if we could bring in a cardiologist, a pulmonologist or other specialist. Dr. Ghannam stated there was no problem with Shannon’s heart, his enzymes were fine and there was no need for additional healthcare professionals as he himself was a cardiac specialist and a pulmonary specialist. He further stated he would not prescribe the steroids requested due to the possibility of elevated blood sugars, increasing the risk of stroke or heart attack.
He then asked, “Your husband was a smoker and a drinker, right?” His question indicated to us he was unfamiliar with Shannon’s medical history and left us wondering whether he had even read Shannon’s chart. Shannon was neither a smoker nor a drinker. Dr. Ghannam stated Shannon’s lungs were permanently damaged and looked like bricks, unable to contract and expand with breathing. He stated Shannon was also being given high levels of Nitric Oxide to assist with breathing.
At that point, Dr. Ghannam again began trying to convince us we had no choice but to put Shannon on Comfort Measures. We asked for an explanation of what Comfort Measures entailed, and then declined, stating that Shannon had already regained consciousness twice in two days, both times indicating he was fighting to live and wanted to return to us. We clearly stated we felt putting Shannon on Comfort Measures as described by Dr. Ghannam, was the same as murdering him and we stressed we wanted to honor Shannon’s desire to live and return to home to us.
Dr. Ghannam and the Care Team continued to aggressively push for us to remove Shannon from the ventilator and let nature take its course, for his dignity. Our older son again confronted Dr. Ghannam and asked why the newspaper had just recently reported that another Kadlec patient, who was considered to be a community leader, was allowed to remain on the ventilator for almost 3 weeks before he was removed, but with his own dad, it had barely been a day and the doctor was already pushing to have him removed from the ventilator and placed on Comfort Measures, to which Dr. Ghannam replied, “Well I guess we could give him a few more hours…” Our older son then asked if I could spend the night with his dad and Dr. Ghannam stated he didn’t see why that would be a problem, but he would let us know. We returned to Shannon’s room to spend the afternoon with him.
A couple of hours later, Shannon again regained consciousness when his meds ran out and he was with us for another 5 to 7 minutes. He was able to respond to our yes/no questions and teasing with flinching and mild facial expressions. For a third time, we asked him if he wanted to live and was fighting to come home to us, and he indicated yes. Once Joshua replaced his IV meds, he slipped away again.
We stayed with him the remainder of the day, talking, and laughing and loving on him. His eyes would water occasionally, and he appeared to be crying. We tried to ask Joshua questions about the drugs being administered and his treatment, but he was evasive and seemed reluctant to explain and often his explanations led to more questions. Many times, he and the other nurses, when questioned about the particulars of Shannon’s treatment, would just stiffen up and mumble something about “the rules”, the “rule book” or “the CDC.”
We were struggling to understand Shannon’s sudden decline and why he was on so many powerful paralytics, sedatives, and pain killers at the same time for so long. We asked about the machine that was monitoring respirations and were told the intermittent orange artifacts that appeared from time to time were his body trying to resume breathing on its own. When questioned about that, Joshua stated the drugs were to keep his body from fighting the machine and the drugs were paralyzing Shannon from the waist up.
Our sons questioned why Shannon’s breathing muscles were purposely being paralyzed if his body was fighting to breathe on its own. Joshua declined to offer any adequate explanations. At one point during this visit, Shannon developed hiccups and that left us with more confusion and unanswered questions. We also asked Joshua if Shannon had been fed yet, and Joshua denied knowing, stating Dietary would be assessing and providing nutrition but no specific details beyond that. Later that day, Joshua said Michelle, Floor Nurse, had authorized me to spend the night with Shannon, but our boys would have to leave when visiting hours were over. Shannon did not regain consciousness again that day, but his vitals were holding, and his condition was stable.
Before our boys left for the day, we discussed Shannon’s situation, and agreed to honor Shannon’s wish to keep fighting as he had indicated a powerful desire to live and return home to us. We refused the frequent offers by nursing to downgrade him to Comfort Measures, “for his dignity.” As Dr. Ghannam had explained the process of Comfort Measures to us, Kadlec would administer higher levels of sedatives and pain medications to Shannon before nursing removed the ventilator and we would be allowed to stay with him until he passed “naturally.”
It was unlikely Shannon would ever regain consciousness to tell us good-bye as Jessica, RN, stated he had indicated as his last wish before Kadlec put him on the ventilator. We were aware and had accepted that Shannon might lose his battle, but we felt we owed him the opportunity to fight based on our recent interactions with him. At no point did we authorize discontinuation of treatment or Comfort Measures, either verbally or in writing.
Paula, Bedside RN, came on shift and began flushing his lines and suctioning his vent, using the built-in sling to reposition Shannon in bed. Other than noting his obvious transition from prone to supine, this was the only time I had witnessed nursing reposition him or perform the routine skin checks prescribed in Shannon’s medical chart. Earlier, I had noticed that Shannon’s NG tube was gone and there was used tubing on the floor behind the bed. I asked when he was scheduled to eat again, and Paula denied knowing and stated Dietary would have to make that assessment. When she saw the used tubing on the floor, she tried to discreetly pick it up and walk over to dispose of it in the biohazard bin.
I never did see or talk to any Dietary Staff. In Shannon’s medical chart for September 3rd, (10:24 p.m.), Paula noted Shannon was NPO, but despite family’s repeated inquiries into his dietary status, Kadlec nursing neglected to make family aware of this fact. Respiratory came in from time to time to fuss with the machines but offered no explanations or insights to his treatment. Paula’s interaction with Shannon was the most hands-on activity towards him I had witnessed from staff in the hours I’d been allowed at his bedside.
She was preparing to administer a full liter of pinkish, sudsy liquid, which she identified as a stool softener, via his IV port, and warned me not to be alarmed if Shannon had a large bowel movement sometime the next morning. I was confused by this because Shannon had not had anything to eat since about 10:30 a.m. on the 1st of September. He had mentioned over the phone that he’d been able to use a bedside commode shortly after eating, and this is documented in his chart. None of Shannon’s nurses could confirm that he’d been fed since, so why the need for stool softener and in such a large amount?
Paula was very clinical and disengaged as she went about Shannon’s care. She did not talk to him or explain what she was going to do to him or for him; there was no warmth to her at all. She would briefly answer whatever questions I had but she wasn’t open or forthcoming and she gave me the impression that she was intently focused on preparing his body for his death, just going through the motions instead of actually providing beneficial treatment and care. She finished what she was doing and told me not to touch or talk to him too much because it was his normal rest time, and she didn’t want him to become overstimulated by my interactions with him.
Shortly thereafter, I met Dr. Phani C. Kantamneni (Dr. K.), the doctor that performed Shannon’s intubation procedure. He introduced himself and told me I did not need to wear a mask. He questioned why Shannon had chosen not to get the vaccine. I explained the situation with our GP and our newly scheduled first available appointments with the Kadlec Residency Clinic. I clarified Shannon wasn’t necessarily against the vaccine; he had questions and wanted to talk to a doctor about his health concerns so he could make an informed decision.
I asked Dr. K about the availability of alternate treatments being successfully utilized such as Hydroxychloroquine or Ivermectin, but he stated he was not allowed to consider any of those treatments as they were off-label, and it was illegal for Kadlec to use off-label drugs to treat Covid. Dr. K started telling me a story about a local doctor that was being prosecuted for prescribing Ivermectin, and I interrupted him to ask why Shannon was still being administered the Nimbex, the paralytic drug that was supposed to be discontinued once Shannon had stabilized in supine. Our family was concerned the excessive use of the paralytic drug may have been working against Shannon’s recovery, and we had not been informed of any medical issues resulting in the need for its continued administration. Dr. K denied having any knowledge of this but instructed Paula to immediately discontinue the Nimbex.
When I mentioned the three instances when Shannon had regained consciousness long enough to communicate with us, indicating he was fighting to come home, Dr. K did not comment but suggested I might have another opportunity to talk with my husband when his Propofol IV drip ran out again in a few hours. Dr. K then asked why Shannon was a Full Code – was I sure I wanted Kadlec to perform CPR on Shannon if he were to code? Dr. K. painted an awful picture of the additional pain and damage, including broken ribs and punctured lungs, which Kadlec would inflict upon Shannon’s already stressed body if staff were required to perform CPR.
Kadlec had not acknowledged Shannon’s code status to me prior to Dr. K’s question, so I did not know Shannon was Full Code and expressed my surprise at this information. From my perspective, at the time, this was the turning point in Shannon’s medical intervention. Dr. K quickly motioned for Paula’s attention, began talking to her quietly and making gestures and then left Shannon’s room. It disturbed me to discover months later, in Shannon’s chart notes, that Dr. K had documented “Wife decided to make patient DNR with no escalation of care.” I had not authorized any such change to Shannon’s code status, verbal or written, and Dr. K neglected to tell me changes to Shannon’s care had even been set into motion at that time.
Within the hour, Shannon was able to expel about a liter of urine and his vital signs began to return to a more normal status. We were optimistic he was making a turnaround since he was no longer on the Nimbex, but our hopes were quickly squashed when his respiratory rate began to climb. Paula contacted Chad Allen, ARPN, via cellphone. After notifying Chad of the change in status, she turned and stepped away from me, covered her mouth with her free hand, lowered her voice, and muttered, “Yes, she’s still here…” She talked with Chad a few more minutes then hung up her phone and left the room. She returned with several vials. When Paula failed to explain what she was preparing to administer, I had to ask, and she identified the medicine as Versed and began injecting them one at a time into the IV port in Shannon’s left arm. She stated it was to help regulate his respiratory rate, and within a short time, it appeared to be working.
On September 4th, around 2:30 a.m., Shannon’s Propofol IV drip ran out but was not replaced. According to his medical records, it was discontinued at that time, but no other information is given. Also, per Shannon’s medical records, dosage for the Fentanyl was gradually increased over several hours until midnight and remained at elevated levels four times higher than initially prescribed at the time of intubation. Shannon did not regain consciousness a fourth time, as we’d hoped.
As I sat with Shannon grasping his hand tightly, and comforting him, several of the staff again gathered at his door to gawk and whisper. I asked Paula to remove them from his doorway and give us our privacy; she stated they only wanted to help but had no explanation how standing around intruding on our space was helping. As the hour progressed, the orange artifacts on the respiratory monitor increased significantly and in a more rhythmic pattern and Shannon’s head and shoulders lurched forward in a bucking motion, his upper torso bouncing up and down on the bed.
His temperature climbed to 104 degrees, but the doctors had insisted there was no secondary infection. Shannon’s heart pounded away at 160 bpm for the last few hours of his life, but Kadlec staff made no effort to address it or explain what was happening to him. With each passing moment, the lurching became increasingly more violent, but the only remedy Kadlec would offer was Comfort Measures. From that point forward, Paula began asking me every few minutes if I wanted to consider changing Shannon’s status to Comfort Measures and I declined each time, telling her he was still with us, asking to live and we felt like we would be murdering him to do so. Nonetheless, Paula remained as relentless as a used car salesman in her attempts to interest me in the Comfort Care Package, “for his dignity,” lest I forget it was an option.
The bucking slowed, then stopped and Paula exclaimed, “I think he’s gone…” then stated she wasn’t entirely sure as the monitor showed he still had a heart rate wavering around 50. She stated she believed it was a residual value that remained because of the ventilator. She pronounced Shannon dead at 4:55 a.m. on September 4th, 2021. In my shock and confusion, I believed I needed to change back into my street clothes and went into the bathroom in Shannon’s room.
I had changed into Shannon’s sweatpants and pajama shirt earlier for the night and I had it in my head that he would need them to leave the hospital. When I returned to Shannon’s room, the ventilator and associated equipment had been removed, but a mass of thick, pinkish-tan foam frothed out of his mouth. When I brought the foamy exude to Paula’s attention, she expressed surprise and alarm and quickly suctioned his mouth. When I asked Paula what caused Shannon to foam at the mouth, she denied knowing what had happened.
I told Paula I was going to call our boys and I’d appreciate it if she would make sure they were allowed up to Shannon’s room. She parroted Kadlec’s strict visitation policy that only allowed for one family member, which made no sense to me as we’d all just been together in Shannon’s room less than 12 hours earlier. I asked her if she were truly, on the worst day of my life, going to make me choose which one of our sons could come up to say goodbye to their dad. She asked me what I wanted her to do about it and I suggested she look the other way.
There was absolutely no patient advocacy going on at Kadlec during this time; only staff’s immense concern for “the rules” and “the rule book.” We were put off from the very beginning, unnerved by the overwhelming lack of compassion by Kadlec staff. They moved around Shannon and his room like automatons, void of any warmth or genuine emotions, focused only on their assigned duties, thoughtlessly indifferent towards Shannon and his family, if they even bothered to enter his room at all. Most of their monitoring was done through the small window outside his room or via computer screens at the Nurse’s Station. The Kadlec ICU, itself, was a cold, dead hostile environment, as if there was no humanity present.
Our experience of losing Shannon while he was entrusted to Kadlec’s care left our family with so many unanswered questions about his treatment at the hands of the numerous medical staff that crossed his path. Where were we supposed to go for compassionate, expert medical care if not the ICU? Who should we have trusted with our loved one in need of life-saving intervention?
What were our options for competent medical care when we were helplessly struggling with a horribly sad situation, distraught over Shannon’s suffering and fielding what felt like was an almost constant urgent need on the part of his Kadlec doctors to be rid of him? Why did Kadlec even bother employing skilled medical professionals if the staff’s only permitted treatment pathway consisted exclusively of “checking the CDC website?” Did this coveted CDC dictate issue Kadlec staff a license to cruelly abuse and gaslight their elderly unvaccinated patients?
Did the CDC’s glorified edicts provide Kadlec staff a green light to terrorize and bully their vulnerable charges into submitting to treatments they may not have understood, needed, or wanted? Did this “one-size-fits-all” prescription written by the CDC enable Kadlec staff to bypass the best interests and needs of a medically complex individual? Did it include nixing the right to try viable alternative treatments as last chance options?
Did this faceless mandate support Kadlec allowing doctors to sidestep the POAs of their unfortunate victims and deprive families of the traditional end-of-life care to which they are entitled? Did it grant Kadlec a permission slip to forego the legally required and properly executed Informed Consent documents authorizing their doctors to perform invasive and potentially deadly protocols? Did this CDC playbook embrace any occasion for the ill-fated beings to get their affairs in order and say their final good-byes to loved ones?
Did any of Kadlec’s adopted medical protocols incorporate grace or empathy or space and time for those in crisis and their families to make peace with their situation? Kadlec treated us as if we were more of an inconvenience and an irritating bother than as the concerned family of an extremely ill man in need of answers and the assurance of competent, specialized medical intervention, all the while the doctors seemed to be in an urgent haste to exploit their next victim.
In the days following Shannon’s death, I requested a full set of his medical records from Kadlec for the Forensic Pathologist we hired to perform his complete autopsy and toxicology screen. The medical records we received from Kadlec were mixed up and jumbled out of chronological order, difficult to follow and understand, and incomplete with several missing pages. There were many discrepancies between the doctors’ notes, test summaries done by other medical professionals and the Forensic Pathologist’s findings. The FP was unable to explain the excessive overdose levels of several of the potent paralytics, sedatives and opioids still present in Shannon’s cardiac blood two weeks after he passed.
Our daughter-in-law reviewed the notes we were able to obtain and found a medication error in Shannon’s chart where the powerful, highly controlled paralytic drug, Rocuronium, that is supposed to be administered only once at the time of intubation, was entered into his chart several hours later, the following morning, by a second nurse on morning shift under Dr. Ghannam, instead of at bedside, as required by law, by the nurse attending Dr. K with the intubation process the night before.
This fact increases the probability Shannon was either severely under-medicated at the time of intubation, which would have been a torturously excruciating, and detrimental circumstance; or over-medicated, which could also have horribly, debilitating, and deadly side effects. Both prospects are incredibly disturbing, nauseating, and heart-wrenching, but could also explain Kadlec’s reluctant attitude towards any opportunity for Shannon’s recovery. The chart notes are also few and far between, with very little actual objective documentation following intubation and placement on the ventilator, the most critical part of Shannon’s hospital stay.
Given Shannon’s original diagnosis of acute chronic hypoxia, we question the legality and ethics of Kadlec’s consistent choice not to involve myself as his POA or his family in any of the crucial life-altering decisions they thrust upon him in his most vulnerable state of confusion and fear. We also question Shannon’s ability to fully understand and make informed decisions at a time when he was struggling to breathe, and we had alerted Kadlec, prior to intubation, of the changes in his behavior. Shannon was usually a solid, patient person, very level-headed and thoughtful, but in the days prior to admission, he had struggled with bouts of anxiety, frustration, and confusion.
In review of Shannon’s medical records, there are no signed Informed Consent documents for either the Remdesivir treatment or the process involved with placement on the ventilator. Shannon chose Full Code status at the time of hospital admission, and no consent was given by his family, written or otherwise, to downgrade Shannon to a DNR, nor was permission given for Kadlec to go forward with Comfort Measures or outright euthanasia.
It was never our expectation or desire for Kadlec to quit treating Shannon or stop trying to save him. We were verbally adamant on several occasions about allowing Shannon the right and dignity to fight for his life. The Kadlec medical professionals in charge of Shannon’s care shredded his dignity by failing to protect his modesty or respect his privacy. Kadlec also neglected to acknowledge Shannon’s basic human rights or honor the promise they made to him before they performed the ventilation procedure. Kadlec’s indifferent attitude and resulting treatment towards Shannon reduced him to little more than a slab of meat.
Shannon had an incredible will, most likely fostered by the frightening confusion and upheaval of his life as a little boy, and as a result he became very resilient to life’s adversities. He possessed a near superhuman ability of mind over matter and we believe, in the end, these were the attributes that kept Shannon fighting so hard to return to the life he loved long after the Kadlec doctors had written him off as “a dead man walking.”
It is our impression that Dr. Ghannam, Dr. K and Chad did not expect Shannon to hang in as long as he did. Shannon’s horrific death has wreaked unbearable injustice upon the world we built around him and it breaks our hearts that his last few days on this earth were filled with so much torment and cold terror, not unlike the first few years of his life. It was an unkind, unfair, cruel and calloused ending to a warm, loving human being with a generous heart and there are no words sufficient to express the pain of our devastating loss.
Kadlec’s gross negligence separated Shannon’s precious grandbabies and his heart, from their favorite “big kid” playmate and forever buddy. Kadlec cheated his boys out of their biggest champion and amazing life teacher. My heart and soul are crushed beyond measure, and the being I was with Shannon, the life we shared and future we had planned together all died with him.
Shannon’s siblings are devastated the baby brother they raised was snatched away before his time. His family and people that love Shannon have lost a solid and dependable ally because of the Kadlec staff choosing “the rules” and “the rule book” over the patients. This tired, depressing world is missing a beautiful, gentle soul and it is not made better by his absence.
But the saddest heartbreak of all, Kadlec ripped Shannon from the fulfilling life he had built; stripped him of the chance to enjoy all the things for which he’d worked so hard; robbed him of sweet memories of joyous adventures and thrilling treasure hunts that could have been, and short-circuited his connection to all the beauty, love and delight for life he shared with everyone he knew. In the last few days of his life spent in Kadlec, it was Shannon’s sad misfortune to wind up reliving his earliest unhappy experiences, confused and afraid, and at the mercy of strangers indifferent to his struggle and his suffering.
Filter By Category
Age: 49
Location: CA
Admitted: 01/24/2021
To: Kaiser
Murdered: 01/25/2021
Raymond Albert Martinez

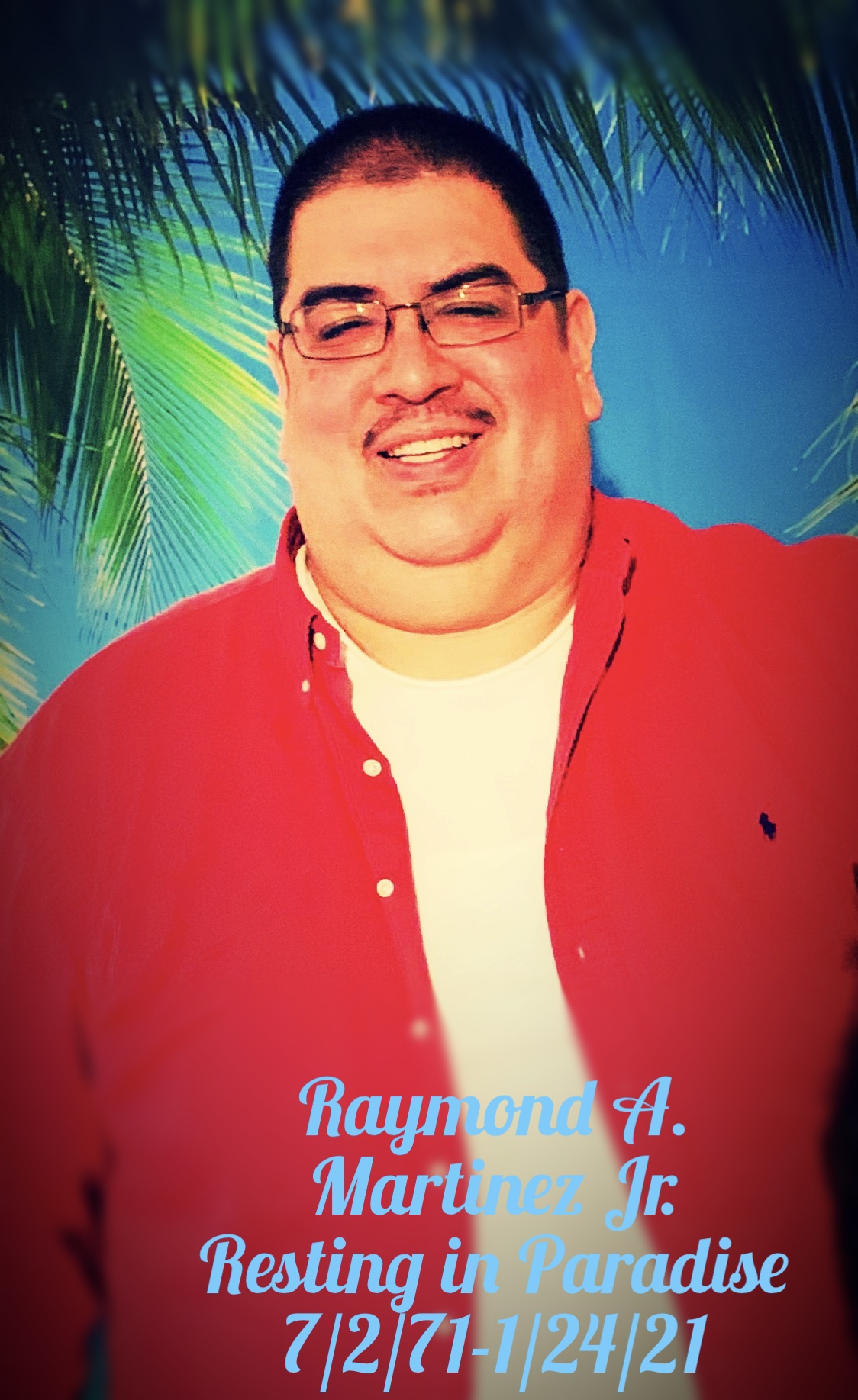
Age: 79
Location: PA
Admitted: 12/07/2021
To: Allegheny General Hospital
Murdered: 12/15/2021
Kathleen Schwab

Age: 57
Location: IL
Admitted: 10/29/2022
To: St Marys
Murdered: 11/19/2021
Dawn Mobley

Age: 29
Location: TN
Admitted: 05/08/2021
To: Leconte medical center and Vanderbilt university medical center
Murdered: 07/23/2021
Kenneth James Anderson Jr

Age: 47
Location: NM
Admitted: 08/26/2021
To: Mercy Medical Center Durango, CO
Murdered: 09/27/2021
Suzanne Moore
Age: 71
Location: MI
Admitted: 10/04/2021
To: Trinity Health Muskegon
Murdered: 10/14/2021
Douglas Niles Wilson

Age: 79
Location: NE
Admitted: 12/27/2021
To: Western Nebraska Regional Hospital Scottsbluff, NE
Murdered: 12/27/2021
Sharon Kaufman

Age: 64
Location: TX
Admitted: 08/12/2021
To: HCA Houston Healthcare Conroe
Murdered: 08/22/2021
Mark Franklin Parkin
Age: 28
Location: TN
Admitted: 09/25/2021
To: Tennova
Samantha CB

Age: 70
Location: CO
Admitted: 11/25/2021
To: Denver Health Medical Center
Murdered: 01/04/2022
Esmegrado Cruz Amaya

Age: 54
Location: SC
Admitted: 08/28/2021
To: Coastal Carolina was the first hospital I took him to on Saturday morning; Beaufort Memorial on Saturday evening.
Murdered: 09/08/2021
Terry Wisdom Jr.
Age: 62
Location: TN
Admitted: 09/06/2021
To: Tri Star Southern Hills
Murdered: 09/22/2021
Calvin Lester Jones

Age: 53
Location: SC
Admitted: 10/23/2021
To: Easley
Murdered: 04/15/2022
Susan Elaine Propes
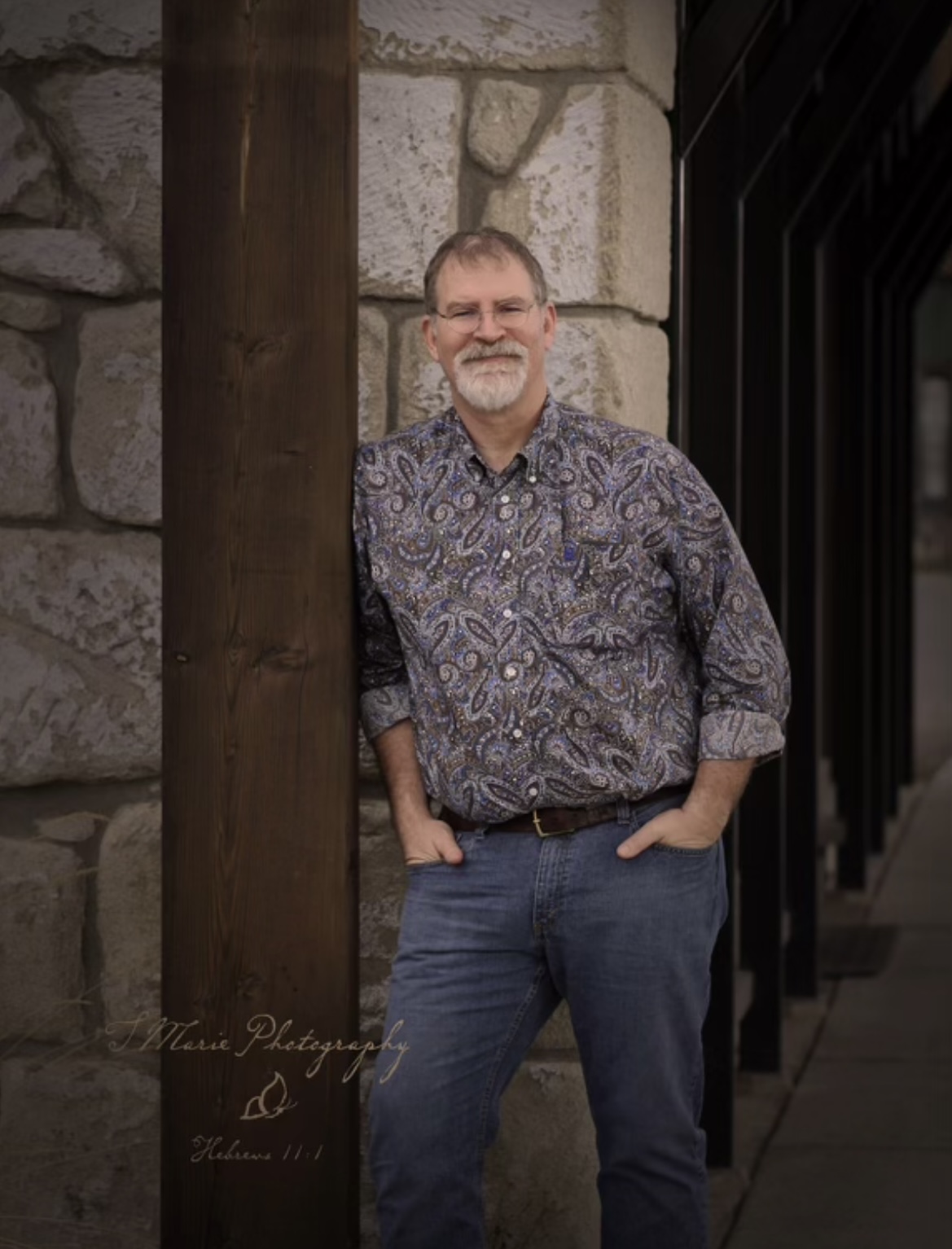
Age: 53
Location: WA
Admitted: 09/22/2021
To: Kadlec Regional Hospital
Peter Weron

Age: 50
Location: MI
Admitted: 09/25/2021
To: Mercy Health
Murdered: 10/10/2021
Nick Percy

Age: 65
Location: TX
Admitted: 07/04/2021
To: Baylor, Scott and White
Murdered: 08/07/2021
Alan Leonard

Age: 64
Location: NV
Admitted: 10/15/2021
To: Mountain View Hospital and Pam Rehab
Regina Bell

Age: 63
Location: CA
Admitted: 12/18/2020
To: Fresno Community
Murdered: 01/11/2020
Barbara James

Age: 43
Location: WI
Admitted: 09/03/2021
To: Bellin Memorial Hospital, Green Bay, WI
Murdered: 10/10/2021
Doug Roatch

Age: 60
Location: MI
Admitted: 04/03/2021
To: McLaren Northern Michigan Hospital
Murdered: 05/05/2021
Paul Kucharek

Age: 61
Location: AZ
Admitted: 07/06/2020
To: Honorhealth Thompson Peak
Murdered: 08/04/2020
Eric Cedarstrom

Age: 63
Location: IL
Admitted: 04/17/2021
To: Northwestern Medicine/ Lake Forest Hospital
Stephen Blackowicz

Age: 97
Location: FL
Admitted: 06/07/2022
To: Baptist Regional Boca Raton
Murdered: 06/11/2022
Janice A. Wallach

Age: 57
Location: CA
Admitted: 08/31/2021
To: Temecula Valley Hospital
Murdered: 09/12/2021
Linda Ann Chappell
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.