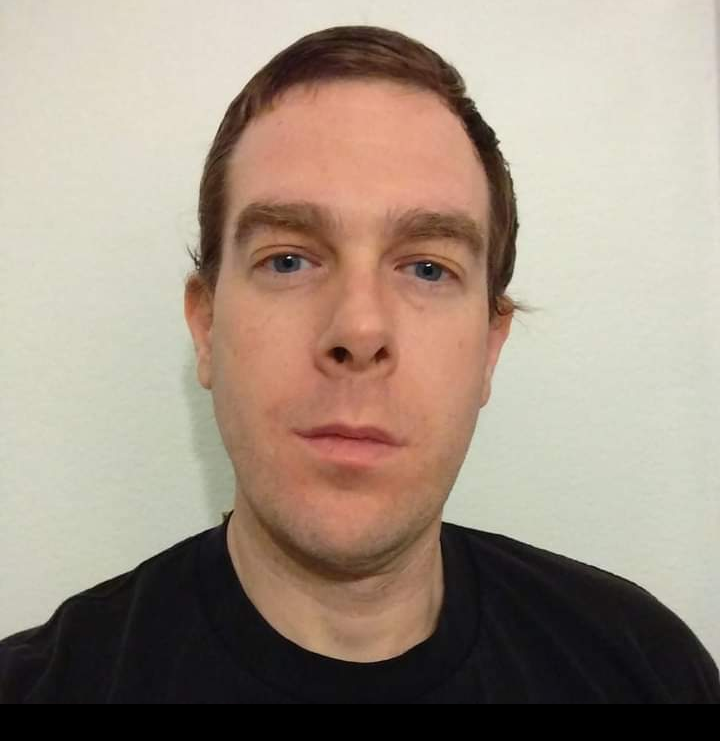
I want to tell you the story of my brother, Michael, a Michigan native who had just turned 40. He was an active person and a talented mechanic who had a love for the outdoors. He had no known health problems. He was in good shape and did not smoke or drink. He was single, without children, and lived alone. He had done extensive research on the vaccines, and the Covid protocols the government controlled in the hospital. I am his older sister, Marie, and Jane is his twin sister along with two younger brothers, Daniel and Greg. We were in charge of his medical decisions, and I was mainly in charge of getting his daily updates from the hospital. Our hospital experience will haunt us forever. We feel his death was the result of a combination of discrimination of being unvaccinated, deadly Covid hospital protocols, and hospital negligence.
Michael Hall had symptoms that began on Dec 7th, 2021. He had a fever, body aches, and started a cough on Dec 10th. By Dec 12th, he was short of breath and it was painful to take a deep breath. He did not want to get medical treatment because of his research, he was afraid to go to the hospital. My sister-in-law went to Michael’s house and checked his lungs for pneumonia. He had pneumonia and his pulse ox was in the low 80’s. My dad convinced him he needed medical care, and drove Michael to the hospital. He went to a small community hospital where he had TWO NEGATIVE rapid Covid tests, and was also negative for influenza and RSV. The nurse said he would probably stay one night and go home with oxygen. Her exact words were “He’s young, he’s healthy, he has no underlying conditions. I have no concerns of him developing severe Covid.” Instead, 24 days later, he died.
Remdesivir and Sedatives
The first day he was admitted, he was given Remdesivir, which we all know Michael had done research on and never wanted! He was given this drug without a positive test. He was isolated from family and had no one there to advocate for him! We were told his chest x-ray showed Covid pneumonia patterns, so it was determined he would receive the hospital Covid protocol. We believe this drug is what put him in the ICU. He went downhill after the first dose and was then on 55L of high-flow oxygen. We felt like he was trapped in the hospital, within 24 hours of his admission. He was requiring so much oxygen, that we felt like we couldn’t take him home. His decline was immediate after Remdesivir. We explained to the nurses, we do not want him on that drug and to take him off. He was on this drug for 4 days and was then finally discontinued. Michael also received on dose of the experimental drug called Baricitinib; however, the hospital would only administer this drug as long as we approved Michael also receiving Remdesivir. So, they made us think there was a new “miracle drug” but they withheld this drug, unless given with Remdesivir. Michael also started receiving a cocktail of Precedex and Morphine, beginning on the first day of his hospital stay. They immediately started a sedative cocktail of medications, that make breathing more difficult. The ICU Dr wanted him transferred to a bigger hospital. They tried to transfer him to many hospitals, and all said they would not take him due to no bed availability. The Dr said he would transfer him to Ascension Borgess, in Kalamazoo, as a last resort but that it would be a “stepping stone” until he could get into a bigger hospital, with more options for such a young patient. The next thing we knew, he was transferred by ambulance to Ascension Borgess on the evening of Dec 16th.
What followed were days of ups and downs, horrible traumatizing phone calls, and what we feel was hospital negligence and mistreatment. He was on BiPAP upon admittance. The nurse’s concern was lack of nutrition. She explained to me over the phone the Drs felt it was too risky to place an NG tube. This nurse told us Michael needed a minimum of 3500 calories, just to breathe. By December 16th, he was on his 2nd day of zero nutrition. The nurse tried to convince the Dr she could get in place quickly and was repeatedly told no. Around 48 hours after the last bag of Remdesivir was hung, he was doing great and showing improvement!! The nurse was able to get him up and marching in place and sitting in a chair off the BiPAP and just the nasal cannula. He was able to drink two protein shakes, which was the only nutrition he had had in days! He had started texting us with sarcastic comments which showed his fighting spirit was back! Even during this time, while Michael was able to remove his BiPAP mask and use a nasal cannula, the Dr still wouldn’t allow the nurse to place a feeding tube. Michael had proper nutrition withheld from him, from 12/15-12/21.
Lack Of Care
That night he suffered bilateral pneumothorax. His day shift nurse called me and told me she left him at 7:30pm after getting him transferred from the chair back to bed and back on BiPAP. The next morning when she arrived for her shift, she found Michael full of subcutaneous air everywhere in his neck and right arm. When asked her opinion of how long he sat with two collapsed lungs, her response was “most of the night”. She said the night shift nurse used the excuse that Michael never hit the call button to say he was in pain!! So, it’s the ICU patient’s fault? Why was he not being monitored? After this incident, everything went downhill. Next were chest tube placements, blood clots everywhere in his entire right upper extremity which led to PICC line infection and removal, and increased work of breathing. The nurse told us he was very close to being intubated and said she could sneak in one visitor. Greg, our younger brother, was able to see him. Michael was alert and oriented when Greg was visiting with him. He was SO happy to see a familiar face. Greg sat with Michael, read him letters that all of his nieces and nephews wrote him, and Michael was laughing at the pictures they drew him. Michael wasn’t able to talk, his throat was so dry from the BiPAP, that he had no voice. However, he did communicate with Greg using hand signals, he laughed, and he held Greg’s hand as soon as Greg walked in the room. The joy and relief of having a visitor for the first time in 9 days, was obvious.
That night, in the early morning of Dec 21, I received a frantic phone call at 3am from the Dr. She said as soon as she intubated him, the force of the ventilator made his left lung pneumothorax bigger, and when she was setting up to put in a chest tube on the left side, the pneumothorax put pressure on his heart and sent him into cardiac arrest. I was told they did CPR for 7-8 minutes until he was stabilized. The nurse called a couple of hours later saying we needed to get to the hospital because he was not doing well. She was able to sneak us in to see him. His right arm was so swollen and purple and full of clots. Later that afternoon, they put him on dialysis. The Dr explained to us “first Covid affects the lungs, then the kidneys next.” After Michael’s cardiac arrest, his cardiac rhythm was occasionally switching between normal and a-fib. The nurse told my sister-in-law, that this is completely normal, and no drugs would be given unless they were worried about the a-fib throwing a clot. The nurse reiterated, that Michael was already receiving the blood thinner Heparin, so the Drs were not worried about the atrial fibrillation. Within two days, they administered a drug called Amiodarone, to convert Michael’s a-fib to a normal rhythm. No one called the family to let us know this drug was being given. This medication should be used as a last resort for ANY patient, but especially patients who are dealing with lung issues. Why? The most common side effects of Amiodarone are lung toxicity! Greg, being a pharmacist, knew this was grossly the wrong medication to give to Michael. We felt like they were trying to quicken his death.
The Push For Death
The care team was concerned with his brain activity after cardiac arrest, so they performed a head CT on Dec 24th. I received a phone call later that afternoon that showed his brain was normal with no sign of stroke or anoxic injuries! We were able to do a Zoom call with Michael on Christmas Day. At this point, we had been told all labs were in good range! We were joyful and full of hope and while on the Zoom meeting with all of the family and kids, a palliative care Dr called me. I asked if I could put her on speaker phone so the whole family could hear. She had an absolutely horrible bedside manner. She proceeded to tell us Michael was in very critical condition and if he went into cardiac arrest again there would be nothing more they could do for him. I told her he didn’t have a DNR and would they even do CPR? She said, ” No, CPR wouldn’t do him any good at this point.” She also stated he could be brain dead, and we should consider getting hospice involved and pulling him from life support. Needless to say, after being on the ventilator for only 4 days, and just given good news about his head CT and labs, we were completely shocked! We all asked questions and she said “I don’t know where the disconnect is, but your brother is on the highest forms of life support and very few make it. The statistics are grim.” She was horrible, had no compassion, and talked down to us all. All of the young kids heard everything, and we didn’t know why she felt she needed to tell us this terrible, non-emergent news on Christmas Day of all days, and on a Zoom call with the patient who could possibly hear everything! In fact, we saw Michael’s vitals on his machine and his heart rate jumped to 150 as she was speaking! After she hung up, it went back down in the 70’s.
The following week we were able to get two visitors approved. Between my sister Jane, and my brother Greg, someone was able to visit him daily. Every time we questioned why no visitors if he never tested positive for Covid? We were told they were going off his first chest x-ray that showed Covid pneumonia patterns as Day1 and after 21 days, more visitors could possibly be approved. Every time we asked if he ever tested positive, we were given an offhand yes answer, without anyone looking anything up in his chart. During this week, my siblings met two very kind, compassionate nurses who treated Michael with care and dignity. One Dr was friendly. The rest of the nurses and Drs we encountered were indifferent, uncaring, or just downright cruel. We were told by the attending Dr for the ICU, that they had six people waiting for his bed. We told them they needed to give Michael the best fighting chance! He is only 40! One evening, as my sister sat with Michael, a male nurse went on a rant about the unvaccinated and said “if these people would have just gotten the shot they wouldn’t be here and they all come in here wanting our help but it’s their own fault”! He was angry. Jane said he came into Michael’s room apologizing that he was so tired as he was “still drunk on Nyquil from a sinus infection.” He was carelessly banging on machines and roughly changing out IV bags. He told my sister “IF he survives this, it will take him forever to get out of here.” Every 12 hours, a different Dr was in charge of his care. We fought for Michael! We asked for monoclonal antibodies, we were told by two different Drs that once a patient is admitted they are automatically disqualified. Why? We weren’t given an answer besides “protocol.” We asked about alternative treatments and medications (my brother Greg is a pharmacist and suggested other drugs he had been researching). Our education level was questioned, and we were told, “don’t get lost in the weeds” regarding different treatments. We asked for Ivermectin, Budesonide (inhaled steroid), and NAC (N-acetyl cysteine AKA Mucomyst). The Dr told us “we don’t know what kind of interactions or side effects these drugs could have, with the drugs we are already giving Michael”. So, we asked why they would give him Amiodarone, when the most common side effects are lung toxicity? The Doctor’s attitude completely changed, and he got very angry. His response was “we are doing everything we can for him, and we’ve already done 4 times more than what we do for other patients!” The same Dr also said that they were giving Michael an inhaled steroid….Albuterol. Once again, we told the Dr that we knew that wasn’t a steroid, and he was angry. We felt like they were constantly lying to us. Had we not had the medical background and knowledge in our family, they would have gotten away with it.
A Turn For The Worse
January 2nd was a great day! Vent settings were down to 75, sedation was lowered and my sister was with him for 3 hours that afternoon. His eyes were open for long stretches of time! She was able to show him Christmas morning videos. The entire family was together on a Zoom call and we saw his eyes open! We were so full of hope. However, when the nurses came into the room and saw Michael with his eyes open, they immediately administered more sedation medications. They would never turn his sedation down and even attempt to test his neurological functions. They wanted Michael fully sedated, at all times! The next day his vent settings were back up to 100. Jane went to visit him that night and Michael was heavily sedated again. She felt the staff was not acting as they normally did with her and were vague in answering her questions.
We had been continually trying to get Borgess to transfer him to a facility with respiratory dialysis or ECMO and other treatments to give him the best fighting chance and were always told they had tried, but no one would accept him as he was not a candidate due to his cardiac arrest. I would call the patient care advocate many times and left several messages and was told she was off for the week and I could not get anyone to return my call and when someone finally did, she was very rude. We still don’t know if any efforts were ever made to get him transferred. On the morning of January 5, 2022, I received a phone call from the resident. I was told Michael’s blood pressure and oxygen levels were falling and this was “the end of the road.” I was completely in shock and asked if we could all come see him right away! There are 8 of us and the Dr. agreed to let 6 of us come see him as he was ‘actively dying”.
I was the first one to arrive with my brother Greg shortly thereafter. The nurse on duty was one we hadn’t yet met. She was a horrible person. She acted annoyed that we were there and roughly helped us put on our PPE. Told us without any compassion that Michael was alive, but just temporarily. As my brother and I were in the room, a resident came in and told us we needed to say our goodbyes and pull him off life support. I asked him what happened?! He had been doing great and opening his eyes and all vitals had been good. He informed me his oxygen had been going down to the 60s and 70s throughout his entire hospital stay and they felt he had no brain activity. I said this is the first we are hearing of this!! We have detailed notes and NOT ONCE were we told of low oxygen levels!! The lowest that had been reported was 85.
Saying Goodbye
All 8 of us assembled in a conference room along with the resident and a palliative care Dr. He gave the same speech to all of us. It’s time to say goodbye. No brain activity. We asked the question: how do you know he is brain dead? He said in his opinion because of the repeated episodes of low oxygen. We said his brain CT came back normal! Dr said his MRI did not come back normal. I said he never had an MRI!! The Doctor said, “that’s right, he couldn’t have an MRI due to his jaw surgery.” We said he had never had jaw surgery and has never had an MRI !! We had totally lost confidence in this team long ago, but this was as if he had him confused by a different patient or were just lying! The care team from day 1, was inconsistent. We felt like we talked to a different Dr every single day, half of them never even stepped foot into Michael’s room or were reading off of the wrong patient’s chart when we would talk with them. We were told if we take him off life support we would all be allowed to go in and say goodbye. The family said we are not doing anything until there is proof he is brain dead. Dr said he would do a bedside EEG to test his brain function. Then we asked if the other 4 family members, who had not seen Michael yet, could go in. They refused. I said on the phone you agreed to 6 people because he was actively dying and now that we don’t want to pull him off life support you are refusing? He said sorry we couldn’t see him. We were only allowed to see Michael, as long as we agreed to take him off of the ventilator. They were blackmailing us! We pushed back. What is the scientific reason no one can go up there? We were told it was hospital protocol. So, we are being punished for not agreeing to give up? Eventually, he gave in and let the other three family members up; Michael’s parents and younger brother, Daniel. Then Jane, his twin, went to see him. She was the seventh person. The same awful nurse refused to let her in. She informed Jane that 6 people were approved to come in and 6 were already up. She begged and said she was his twin, what is one more person? The nurse refused to let her in!
We stayed at the hospital for another couple of hours. We all drove home after the updated phone call stated no changes. Before we left the hospital, my sister-in-law called up to the ICU one last time and asked if the final visitor could say goodbye, before everyone left. You guessed it, the same nurse answered and with the same response “you’ve already had your 6 visitors”. A winter storm had started. As soon as we all got home, one family being 40 minutes away, we got a phone call saying Michael went into cardiac arrest and were told we needed to come up there. The same person who just refused to let Jane in 2 hours earlier. None of us would have made it back in time. He died alone without us. That same nurse actually had the nerve to say “well, I just wanted to give you all chance to be in the room with him, so he didn’t die alone!” We had been sitting in the hospital waiting room for hours, not allowed to see him. The whole thing felt like we were in the Twilight Zone.
The whole experience was nothing short of a nightmare. The next day the kind funeral home director said to us “Michael is in good hands here.” We started crying because not once during Michael’s hospital stay were we ever told this. We blame the hospital for negligence after withholding nutrition from Michael for days. We blame the hospital for negligence after he sat most of the night with two collapsed lungs, and then went downhill from there. We still wonder why he was treated with the poisonous Remdesivir when he never had a positive Covid test and did he ever consent to this drug? He needed his family to advocate for him. It is inhumane to make a patient suffer alone without any support.
Thank you for reading Michael’s story. He was the most kind, humble human being and he had hopes of getting married one day, and having a family. The murderous hospital protocol took that all away from him. It took away an amazing brother, son, friend, and loving uncle. There are so many people left with a giant hole, because his life was cut short. He did not deserve this. No one deserves this.