Murdered
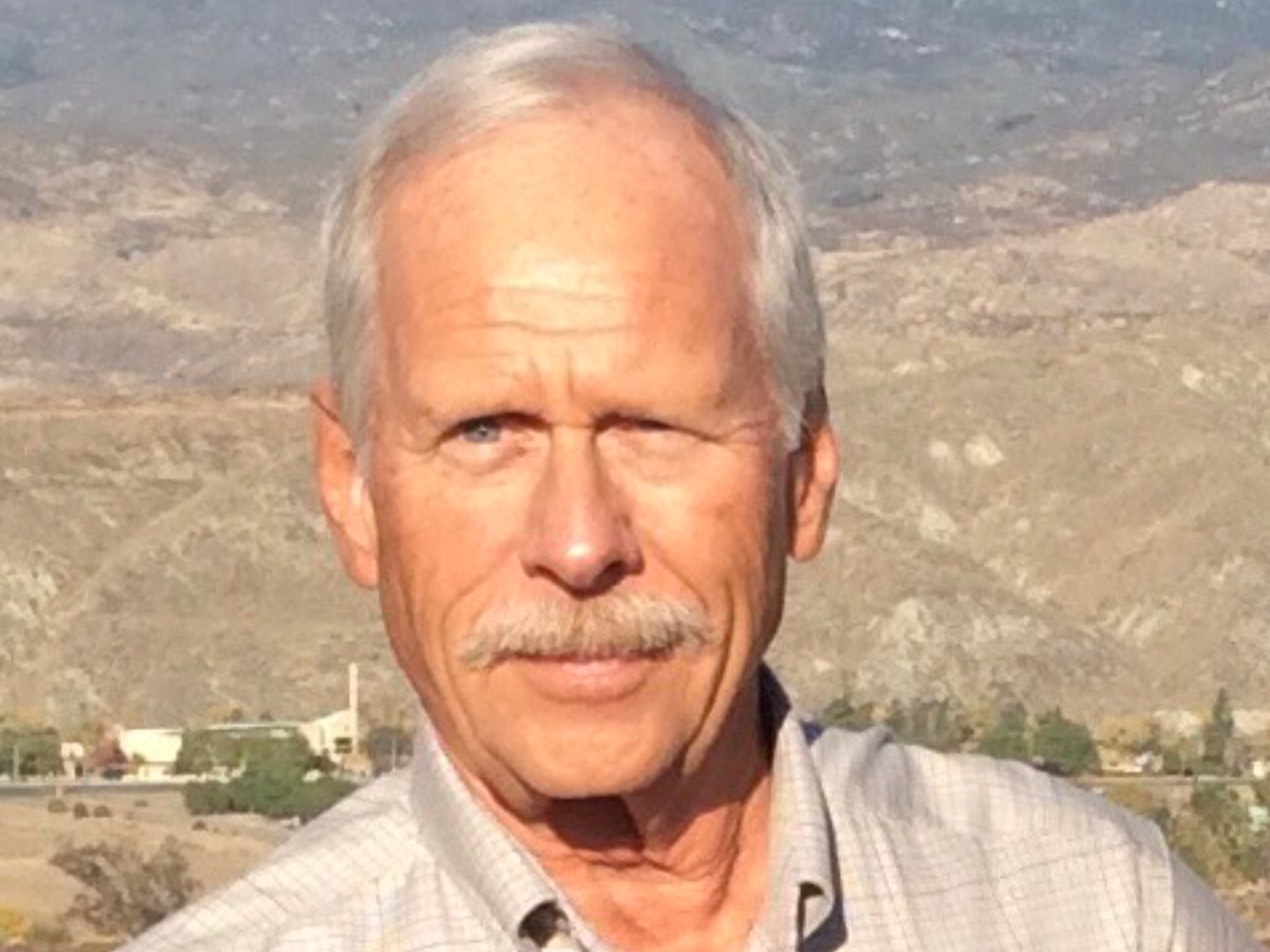
Age: 67
Location: MT
Admitted: 10/30/2021
To: Providence St. Patrick’s Hospital, Missoula, MT
Murdered: 11/13/2021
Martin William Maclay


Denied food and water, pushed the ventilator on her, denied other treatments, was left on stomach where she developed life threatening bed sores.
Christy is a devoted wife, and mother to 5 beautiful children. This story begins early October when she contracted COVID during her pregnancy with Caleb. Matt, her husband will be sharing journal entries, a day to day account of her status, treatment, and care she’s received from Magee Women’s Hospital in Pittsburgh, PA which is a UPMC facility. It’s a long read. If this story touches your heart, we simply ask you share the story with your family and friends to spread awareness of how corporate medicine REALLY treats their patients and families. Some of the staff’s names have been deleted to protect their identity and prevent retaliation against or from the hospital.
My name is Matthew Cresto and my wife is Christy. Before we begin, I would like to make very clear that I have the utmost respect for the majority of the nursing staff here at Magee, giving my wife the best care they can with the tools and options allowed to them. There’s a couple bad apples in every bushel, but the good ones, you know who you are, I can’t thank you enough for your kindness. On with the story. She started showing symptoms of COVID-19 somewhere around October 4th, 2021 and on October 8th late at night, I drove her to Magee women’s hospital as her breathing was becoming labored and at this point she was between 35 and 36 weeks pregnant with our 3rd son, Caleb Samuel. Upon arriving, she was rushed straight to the OB ICU unit on the 2nd floor of the hospital. After getting her settled in and setup with some oxygen, they tested her for COVID. Once her test came back positive, they began talking to us about delivering Caleb ahead of schedule. He was due November 16th according to our math, so this concerned us because he would be premature. The hospital decided to do an ultrasound to get a better determination of gestational age and upon reviewing the measurements taken from the ultrasound, they decided Caleb was actually 38 weeks and roughly 8lb 9oz. This would become the first of many lies from the hospital staff. We then asked if because she was COVID positive, if they would take him from us as we’ve heard horror stories about this at other hospitals. The nurse assured us this was NO LONGER hospital policy and they would not take him from us and he could stay in the room with her since she contracted COVID while he was still in her womb (lie number 2). With this information, we agreed to deliver Caleb. Once Caleb was delivered, Christy and I were able to hold him for about 10 minutes, and then they laid him in the bassinet in the room. There he waited for 2 hours before the Pediatrician came to see him for his newborn exam. He was not 38 weeks, and he was nowhere near 8lb 9oz. Caleb was born premature at 36 weeks, 6lb 5oz, exactly what Christy and I suspected. There was no pediatric staff members there waiting for Caleb.
They said they wanted to take him to the NICU just to give him a good look over and some observation. This is the last time we saw our newborn son until the day he was discharged from the hospital. A couple times a day for a few days, we asked when we could see him again, when she could breast feed him, as they kept telling us as long as Christy wore a mask, she could breast feed(lie number 3). He never returned for feedings, instead they brought in a breast pump so she could pump her milk for him. Before we go any further, I’d like to make note of the extremely LOOSE PPE policy in the OB ICU. The whole time I was there with my wife, not once was I asked to put on a mask, gloves, or gown while in the room with my wife. This was fine with me as I don’t particularly believe they work anyways. During Christy’s stay in the OB ICU she was given 1 dose of Remdesivr, 1 dose of Sarilumab, and steroids to try to fight the COVID, that’s all.
Christy was moved up to the Adult ICU and I immediately knew something wasn’t right. I was stopped outside of her room and told I had to put on 2 layers of gloves, gown, face shield and face mask before I could even enter the room…completely different than the OB unit. After our numerous attempts to have Caleb brought back to us and no resolution, I began to question their motives. This is where things got bad fast. I quietly asked the nursing staff “If I wear all of this stuff downstairs, can I please go see my son”. The nurse contacted the NICU for clarification and 10 minutes later I was informed that not only could I not go see my son, I was not permitted to see him until I have quarantined myself away from my wife for 14 days since I was exposed to COVID by being around her, the same COVID he’d already been receiving antibodies for while he was in her womb. I was crushed and the nurse was so kind as to inform me of this IN FRONT OF CHRISTY who’s now hysterical because her worst nightmare has come true, they confiscated her child and is now keeping him hostage from us. Thanks guy. The best we could get was a low quality web cam live stream of our son in an incubator (nicview.com). The parent bond experience has now been stolen from my wife and child.
Two days later, I was informed that Caleb would be ready for discharge on Thursday, October 14th and that I could pick him up myself, but he was not allowed back to see his mother. What happened to 14 days? It was too dangerous for me to be around him before, being around my wife every day, but now they’re fine with it? Instead of picking him up myself, Christy’s mother (Holly Daum) offered to pick Caleb up instead so to avoid any further backpedaling from the hospital and them possibly keeping him from us even longer. They permitted me to visit him before Christy’s mother picked him up so that I could at least see him and hold him. Mind you, I had JUST LEFT CHRISTY’S ICU ROOM. By now, Christy has been taken off of high flow oxygen and put onto a BiPAP machine which is the last step before a ventilator. Her doctor, the ICU Medical Director, Dr Murugan, comes off as very pushy and ventilator happy, already suggesting we should put her on a ventilator…why?
Now with Caleb and the rest of the children safely under Holly’s care(who’s also a UPMC Nurse and COVID survivor May 2021), I was able to focus on being with my wife. At the advice of Holly, We requested a consult with a Pulmanologist. Later that day, I had to ask again about the consult to which we were answered with “we’ll have to check into that for you”. The next day, Dr Murugan returns to explain his position and why the ventilator should be used, and at our request for him to treat Christy’s asthma, he said rudely, “No, it wont cure covid so there’s no point”. I argued with the doctor that I still wanted to speak to a pulmonologist and he very confidently replied “The Pulmonologist is a buddy of mine and will tell you the exact same thing.” I don’t care, I do not accept your visit as a consult and I demand to speak to a pulmonologist. He also told us that she’s already receiving all of the COVID treatments they had to offer and “Trust me, we’re doing everything we can for her” and that “All upmc facilities follow the same COVID protocol”. Holly can attest to the fact this is not true. Two nurses came in after the doctor’s visit and explained to us that Dr Murugan is “well versed” in pulmonology, though he never identified himself as one. I again had to reiterate that I don’t care who he is, he’s not the person we requested and I demand to speak to that person. The nurse said they would arrange it but they wanted to bring a respiratory therapist up first. Sure, why not. Coincidentally, this is one of the same doctors that delivered Caleb down in the OB ICU.Worth noting: I didn’t hear it myself, but Christy said he tapped her leg and called her his “case study” and told me that she’s not a lab rat.
The RT that came agreed to a liquid form of Combivent, but stated she won’t get much out of it since she’s so short of breath.
October 15th. Dr Murugan came to visit again. I watched him walk into the room wearing all of the appropriate PPE, talked with us for about 10 to 15 minutes, and after making contact with my wife physically, rubs his gloves with hand soap, then walks out of the room wearing all of the same (now potentially contaminated) PPE, converses with the nursing staff in the hallway, touching things, and then walks into another patients room across the hall from us wearing all of the same PPE, never changing any of it. Staff is supposed to remove ALL PPE and dispose of it in the patients room before exiting and then they are supposed to sanitize their hands once outside the room before continuing on. This would not be the only time I watch this arrogant doctor do this. I’ve just been informed at 8:30pm that I’m being forced to leave because of visiting hours. Christy is terrified to be left alone. I was told an administrator would be down to explain to me why I need to leave. At 9:45, Jennifer Pribanic, AOD walks in Christy’s room and asks if I have everything I need, now anticipating to be escorted off the property. She then goes further to ask if I need any pillows or blankets. Caught off guard, now I’m confused and I said this is a completely different conversation than I was left with a little bit ago. She assured me that I was not going to be made to leave and that given the entire situation so far, I’m free to stay for as long as I need and that I needed to be here with Christy. FINALLY someone with some sense here! Jennifer asked me if I needed to order food, then noticed it’s past business hours for hospitality and offered to go grab me some food from downstairs anyway. The first kind gesture we’ve seen from Magee.
Wake up the next day and Christy says her chest doesn’t feel as tight and easier to breathe. Doctor has agreed to give Christy a multivitamin since she was taking a prenatal vitamin already before she came here. FINALLY we get to meet the Pulmonologist! He is willing to try a few more things that so far Dr Murugan has refused and 100% agrees her asthma needs to be addressed as COVID will make it worse. He also adds nebulized steroids to her regimen on top of whatever she’s already getting through IV and she may request liquid Albuterol every 2 hours. Nothing more to report this day.
October 17th. Christy was able to eat a normal breakfast using the high flow nasal cannula with oxygen saturations staying in the 80s. Dr Murugan visits again. He again wears the same PPE in multiple patient rooms…how is this ok?
October 18th. Noon time and Christy is being switched back to the high flow cannula for a break from her BiPAP mask. Up to this point, every time they switch her, they turn the heat up on the oxygen machine so that it doesn’t give Christy a brain freeze. Every other respiratory therapist so far has done this without question and upon request. The young girl that came in refused to do so and because of this Christy became uncomfortable and strained to be able to breathe properly. As her nasal passages felt like they were being frozen, her oxygen saturations dropped into the 70s and I had to loudly yell at the respiratory therapist to turn the heat up as it was HURTING Christy to not be warmer. This girl kept insisting it’s the same setting as the BiPAP which I had to yet again yell and explain EVERYONE ELSE turned the head up with the was NOT on the BiPAP because it was too uncomfortable for her. Finally she complied but the damage was already done. Christy couldn’t recover and her oxygen stayed around 70% and she missed her opportunity to eat lunch. Christy’s now quite angry and it takes the rest of the evening just for her to recover from this mishap and the gross air leaks coming from the improperly fitted BiPAP mask. We were told that an acceptable Patient Leak (PT Leak) was as high we 100L/min. This is the last time we would see this respiratory therapist. We’ve been watching the PT Leak as it rose to over 140L/min and she never returned. To give an example of how bad the leak was, I could see around the mask looking down Christy’s nose on either side. Christy’s oxygen levels never went higher than 80%. Now 7:30pm and the new RT comes in to check on Christy. His name is Denny. Denny is VERY good at what he does and quickly identifies the issue and within minutes the leak goes from 140+ down to <10. Thank you Denny. I made sure to convey my gratitude for him being there to others the next morning.
October 19th, 9:56am. It’s a new day and Christy is now starving from missing meals yesterday. We call down to order food for the both of us and we’re informed that Christy is on a liquid only diet? Must be some mistake. The person on the other end checks to make sure, and yep, her diet was changed 30 minutes ago… I demanded to know why from the nursing staff and <nurses name omitted>, bless her heart for dealing with my now overly obvious anger informs us that because of her poor numbers yesterday they decided to put her on the liquid diet so she could stay on the BiPAP mask more to see how she does for the day. Never mind the fact that her condition yesterday was the cause of a neglectful rude staff member. I refused to eat in front of Christy, so we both went without food for the day, even though she insisted I eat something. Christy refused the liquid diet and because she was upset, she just sat staring at the clock all day long, waiting for what torture they’d introduce next. She looks like she’s just giving up, hopeless, like they’ve taken everything away from her. After some heavy discussing between the two of us, she was back on board and turned her anger and frustration towards the doctors that were punishing her and did everything she could to prove them wrong about her. I’ve had enough. It’s time to get some more concrete answers. I asked the staff what is it going to take to get Caleb in here to be with his mother so she could have SOME glimmer of hope. No decisions quite yet, but they would let me know ASAP. This request was made with the new Attending Physician, Dr Preus.
October 20th and we have one of her favorite nurses again. The nurse looked over everything and had a talk with the Attending about Christy and her limited diet and was able to get them to give Christy back her old soft foods diet, wonderful news. She would let us know as soon as the diet is switched over. They’re going to have a meeting at 1130 with me in the family lounge about Christy. We have the meeting and everyone seems to be on the same page for the most part. Administrators and patient relations seem more apt to trying to help out. I don’t have much to ask for at this point other than getting Christy fed and making sure that whoever switches her over from the BiPAP to the high flow, that they warm the air up BEFORE making the switch so that she doesn’t have a hard time breathing and drop. Everyone agrees, but her oxygen saturations need to be in the 90s before they will allow her to eat since she always drops when they switch her over to the high flow. Finally around 3:45pm they give a little and let her eat, so we order her a dinner plate and they give her some OJ to drink in the meantime, she immediately starts to feel better. 4:30 her plate arrives and she cleans the entire tray. Also Dr Preus has received word back from Infectious Disease and the NICU regarding letting Caleb visit. We originally presumed he could come on her 21st day after the start of symptoms which would be around the 25th, but they decided on 21 days from positive test which would be the 28th, with the stipulation that if Christy’s condition declined and the ventilator became a likely scenario, that Caleb may be able to come in sooner so she could at least see him before that would happen. OK, that’s acceptable. 1 more week.
Next day I head home to take care of some things at home and grab some more supplies/snacks/drinks. Christy texts me that she’s being ignored all day and that they didn’t give her the call button which is supposed to be used to call in case she needs something or needs help. At this point she’s already tried taking her leads off so it looks like she’s dead and nobody’s come in at all and she needs help calling in a food order. I call the Nurses desk and the girl that answers tells the nurse to go to her room to hand her the call button. 20 minutes later Christy texts me again sending me a picture of the call button sitting on the shelf next to the bed out of reach. What is going on here??? I call back and the girl says the nurse already went into the room and gave her the call button and says my wife never mentioned anything about ordering food…..cool so the nurse is lying about taking care of my wife? The rest of the day was uneventful so nothing else to report here.
October 22nd, 6 more days until Caleb can come meet mommy. Christy’s oxygen saturation is up to 98/99%, outstanding! She sat up more than she was ever able to before, allowing the weight of her body to pull her diaphragm down to get more oxygen in. She feels great. The plan was to possibly start weaning down the settings on the BiPAP machine, but she dropped a little this morning due to having to roll a lot to go to the bathroom. The beeping from the monitors was giving her small anxiety attacks, so the nurses set it so it would stop alarming inside the room and only out in the hallway for them. Nothing else to report today.
October 23rd. 100% oxygen saturation! Wait, never mind, back down to 90, and now her heart rate and blood pressure are up. Complains of groin burning and pain lower back around kidneys. They take a urine culture and want to take blood cultures, but at this point she’s been poked and prodded so many times she refuses the extra needles. They give her antibiotics anyway. She’s back up in the mid 90s even while trying to carry on conversations with the BiPAP mask on.
October 24th. They tried to get her situated to go to the bathroom again and she dropped down into the 50s and had a really hard time recovering. I was originally going to leave early in the morning to head up to Holly’s to pick up the kids as 2 of the boys had doctors appointments on Monday the 25th, but I couldn’t leave until she was OK enough. I asked Dr Preus if that exception could be made so Caleb could come see his mother because I was concerned how many close calls she had left before she just couldn’t do it anymore. He agreed it might be time and began contacting the other departments for consideration. I would already have the boys later, the plan would be Monday after the doctors appointments to take Caleb in and the rest of the kids would stay home with my parents watching them. I got word from Dr Preus that because she improved later in the day, they decided to hold off to see how she did, so once again the plan was pushed aside and having the kids, I was unable to return to see Christy that night.
October 25th. I take the boys to the doctors office and everything goes well. Update Christy on everything with the boys and I spend the rest of the day with them at home. Video chat with Christy around 11:30pm, she looks good. Alert, responsive, talkative. This is the last time I’d get to talk to her for a while. (as of 11/21/2021 Christy is still sedated and not recovered)
October 26th, I wake up to 3 missed calls from the hospital. It happened, at 7:30 they decided to put her on the ventilator because when they tried to get her situated to go to the bathroom, she dropped way down into the 20s and couldn’t recover. My heart sank. I call the hospital and talk to the nurse practitioner and he says she went willingly as long as she was fully sedated, to which they complied. I call my dad and rush to the hospital as fast as I can.
October 27th to present. With the help of friends, we quickly go to work searching for treatments, medicines, anything that can help her. We found tons of studies on Ivermectin on the Clinical Trials worldwide database, effects of Vitamin C and Quercetin, effects and direct correlation between Vitamin D deficiencies and the length and severity of COVID, and benefits of ZINC, all being NIH publications and I bring these up to the doctors here and they all decline everything stating that none of it will help her and that it’s a waste. I even offered to PAY OUT OF POCKET and they still refused all of it. I’ve never felt more useless in my life. Completely hopeless and helpless to help my wife. I tried invoking the Right To Try law of 2018 and was met with the determination that it was “written for a different era” and that it doesn’t apply to COVID. Even worse, Dr Murugan, Dr Gosman, the Vice President of Medical Affairs, and Elizabeth Dubovi of Patient Relations ambushed us in a “family meeting” and of course we immediately refused to meet with Dr. Murugan as we are now convinced he’s trying to kill Christy. Dr Murugan leaves the room and we’re informed that if we want to have a clinical medical discussion that he has to come back in, if not then we will talk about options for having Christy moved to another facility. The VP of Medical Affairs refuses to have a medical discussion? We’re also informed that should we decide to transfer her out, she is not welcome at ANY OTHER UPMC FACILITY. Basically we are slapped with an order to deal with Murugan who has a serious God complex, or get out. Elizabeth and Dr Gosman declined to having the discussion recorded. We come to an agreement that Dr Murugan is to stay out of Christy’s room and have no direct contact with her or myself, since there would be no other physician made available to us while Dr Murugan is on duty.
I asked Elizabeth to print out some of the studies we found on the vitamins, thinking maybe if the staff read over the NIH publications that it may sway them to reconsider giving Christy extra vitamins. We were met with a hard no once again from Dr Murugan. I was seen by Heather, Nurse Practitioner and Amber, Nurse Lead and I pleaded my case to them, told them again that I will pay out of pocket and that I wanted the doctors refusal of a reasonable request IN WRITING. Heather agreed with me it was a reasonable request just to check her vitamin levels and agreed that if her levels are depleted, there should be no harm in correcting them. Later that day, I see the lab tests for Vitamins A, B6, B12, D3, and E all listed now which means someone signed the orders for them. Hopeful that maybe we were getting somewhere, I later found out it was Heather that signed the orders, not Dr Murugan. Don’t care, still the result I wanted for the day.
Next morning, I’m met by Heather and Amber again, this time with a completely different attitude. I was informed that they would not be supplementing her vitamins regardless of what her levels are because that’s “not something they do”. I didn’t give much of a response as I realized I lost the last battle I had to fight. She literally signed the orders just to shut me up. Faced with the hard truth that my wife might die because nobody with decision making ability gives a damn about my wife and wants to deny her simple basic medical care. I later get Heather alone in Christy’s room for clarification. She agrees with Dr Murugan’s decision not to treat depleted levels. I’m speechless. This woman had the audacity to lie to my face last night and give me false hope. She later catches me out front waiting on my dinner to arrive. I don’t remember what she was saying as I completely ignored her. She then patted me on the shoulder as she was leaving and it took everything in my being to not tell her to not touch me and to get away from me.
October 31st, Halloween. I’m supposed to be trick or treating with my kids, and where am I? Still at my wife’s side even though she’s fully sedated. Why am I still here you ask? Because I’m so terrified that I’ll get a phone call that she died under Dr Murugan’s care that I can’t bring myself to leave. They’ve successfully robbed me of another life experience with my children. Awesome. Also to note, Christy has been running a fever around 102* for a week straight. Infectious Disease came down to see her and switched up her antibiotics and determined she has some form of fungal infection and bacterial infection.
November 1st. Night nurse, <name omitted> confirms that she’s heard from most of the staff that Dr Murugan “is a prick” and can not believe that they’re withholding simple vitamins from Christy.
Worth noting, Every day we get a “Daily plan of care” that’s printed out. Every day it says they’ve ordered compression sleeves for her legs to prevent blood clots. it reads as follows:
“My Blood Clot Prevention Device is: Sequential Compression Device (SCDs)
Your doctor has ordered special leg sleeves (SCDs) to help decrease your risk of getting blood clots. It is important that you wear them at all times when in bed or as ordered by your doctor. To prevent falling, call for your nurse to remove your SCDs before getting up to walk.”
She hasn’t had them even once, nor have they ever been discussed with us, and now they think because of one of her lab results, that she may have a blood clot somewhere.
November 3rd, Today I met with Bill (RT Director) and a Physicians assistant to discuss the risk/benefit of flipping Christy onto her back again, knowing she did not tolerate it well the last time they tried. We all agreed they had to at least try because they need to be able to check her skin for sores, blisters, rashes, and scan her limbs for blood clots since that was now a concern. While they were in the room, I brought up a few concerns with them. First, the last of the SCD’s that are on the daily care plan, but more so, why nobody has verified that the information on the daily care plan is correct and accurate. I asked if anyone actually reads what they print out, and nobody could answer. This doesn’t sit well with me. I told the PA that I had already asked the other members of the nursing staff around 5 times looking for clarification to no avail and she seemed very surprised as this is the first time she had heard of the issue. Bill suggested if I wasn’t getting an answer I could have reached out to him as well and he would look into it, to which I simply responded “after asking 5 people, i’d assume that I wouldn’t have to contact the director of a department that has nothing to do with the question needing answered. He agreed. Adding to this, I shared my concern about what happens if she has clots and the devices that were designed to prevent those clots were never used even though they’re on the paperwork saying they were in use. The PA said she would look into everything and get back to me. It’s now night time, going into the 4th and Christy is doing very well on her back. Oxygen saturation staying in the mid high 90s, temperature is slowly coming down, as is her heart rate.
November 5th, a new day, a new attending physician. Dr White seems like an OK individual. Dr White has removed the leg sleeves from the care plan since they’re not being used and said that the Lovonox she’s on is more than sufficient to prevent clots (though they confirmed she has a superficial clot in her arm). I gave him an NIH article about NAC and though he said he read over the article, he dismissed it as something to be done very early on with covid and would not help at her advanced stage.
Holly talked with Rob, one of the Nurse Practitioners about some of Christy’s compression sores from being prone for so long, giving specific doses for the vitamins she should receive to aid in wound healing. Rob and Dr White did not object from a wound care standpoint.
Nothing exciting over the next few days. No real improvements to speak of.
November 8th. Christy was doing fairly well all things considered. Her oxygen saturation had been staying in the mid-upper 90s with less than 100% oxygen from the ventilator. Randomly her saturation dropped to the high 70s to low 80s and didn’t move. The nurse today wasn’t as attentive as others and also didn’t give her nearly as many bolus of sedatives when Christy was fighting or out of sync with the ventilator. It took all day for her to get back up into the 90s. It seems harder and harder for her to maintain since they took her off the Phenobarbital. Also today we met the new attending for this week (yes another). This attending is about on par with Dr White, her name is Rachel. She agreed to look over the NAC article as I felt Dr White just dismissed it without reading it, and then said she would send it over to the therapeutics committee for review. Around 9pm or so I hear a buildup of fluid in the tubes coming from the ventilator and Christy’s breathing is very fast, close to 50 breaths per minute. Denny comes in and opens where the tubes meet the tube going into Christy’s mouth and drains out the fluid and her breathing slows down immediately. Apparently a buildup of fluid can trigger the ventilator into thinking she’s trying to take another breath when she really isn’t, causing it to force another breath. Good to know.
November 9th. I was invited to join in rounds and they discussed the plans for Christy. A few topics we went over. We discussed the possibility (or lack thereof) of lung transplants if her lungs can’t recover. No hope there, she has to recover first. Discussed what needs to happen for her to have a tracheostomy. Again, she has to recover first. Rachel is concerned about her constant fever and pointed possibly to the central IV line in Christy’s neck. Suggested a midline instead. I advised Rachel that I had already suggested that and that’s when they put in the PICC line instead. Rachel suggested taking out the central and putting in a normal IV line and I advised her that was a terrible idea as Christy has very small veins and IV lines do not last long at all for her. Rachel mentioned possible infection from the line which I pointed out they drew blood cultures just yesterday and she agreed to wait to see what those look like or if the site of the line starts to get red. They decided to remove another sedative, Ketamine.
It’s around 1PM now. I hear a buildup of fluid in the tubes again. This time I grab the nurses to have it drained before it becomes an issue. The nurse instead of opening the tubes to let the fluid out, lifts the hoses to make it flow back down to the machine. As soon as she does this Christy begins a 2 minute long coughing fit where she stops breathing. I believe some of the fluid wet down into Christy’s lungs. They get her suctioned out, give her 2 bolus of Fentanyl and a “push” of “Rock” which is the paralytic they use to stop you from breathing on your own. This wouldn’t normally concern me except the nurse received a phone call from I don’t know who, but she told the person on the other end that they weren’t in the room and Christy randomly dropped into the 50s, completely leaving out the fluid in the tube and how she drained the tube. A little white lie, but a lie none the less and it makes it sound like Christy just randomly started to desaturate.
I’ve now seen at least 4 times today where Christy shows signs of becoming conscious again. The ventilator starts alarming and then I see Christy’s jaw moving, nostrils flaring, and once i saw her eyelids start to open slightly. Every time they have to give her more Versed and more “rock”
November 11th and 12th. I had to go home the past 2 days to take Caleb to his 1 month checkup. First actual good news in a while, he’s perfectly healthy. He quickly caught up to where he should have been at full gestation, now 8lb 6oz, 20.5″ long, almost exactly the same size as Collin at birth, and almost on his due date. Christy unfortunately hasn’t had as good of news. They removed the Versed and put her back on Propofol for sedation. She is stacking her breaths more now so her saturation isn’t as high as before. Vent settings now 18peep at 100% oxygen, barely holding saturations in the upper 80s throughout the night. This morning thankfully her breathing calmed down some and she’s back up to 91-92, but still not as good as previous days.
It’s amazing what you find out when you look through medical records. I requested a copy of all treatments and medications that Christy has received so far and received it last night. According to UPMC COVID protocol, the proper course of Remdesivir is a 6 day course beginning with a 200mg dose, followed by 100mg each following day for 5 days. She received the first 200mg dose and then every subsequent dose was marked “Not appropriate at this time”. So on top of them refusing any other kinds of treatment, they didn’t even finish off the one treatment that they did offer. So much for “We are doing everything that we can for her”
Dr. Betsy Eads, a Frontline Doctor reached out to me this morning with some things we need to be doing and demanding. Hopefully it helps because this hospital is killing my wife.
Tonight they came in to try to replace her central line in her neck with another picc line in her right arm. The ultrasound nurse did an ultrasound and couldn’t find one of the veins they usually use, the second vein was way too small (surprise surprise) and the 3rd while big enough already carries a higher risk of clotting because of it’s location and how it routes through the shoulder area. This coupled with the fact she already has a clot in left arm, puts her at even higher risk of clotting more and the IV nurse told me that she could place the picc no problem, but she’d be really upset for Christy if she had to come back in 2 days to remove it because it clotted so fast. Christy’s nurse confirmed there’s nothing wrong with the central line, they just want it out as it’s a possible source of infection. The Resident again was suggesting a normal IV but the IV nurse highly advised against that for a couple reasons. She has tiny veins and standard IV’s will fail for Christy, and Propofol is an irritant and would cause burning sensation in her arm since there isn’t enough blood flow to quickly dissipate the medicine. Thank you to the IV nurse for sharing that information. I guess they’ll have to try something else.
Something to note, they keep checking her glucose level, and she’s consistently in the 160-180 range. I questioned this, being that I’m diabetic and I know what range I stay in and what a “normal” human is supposed to be. I was told 160-180 is perfect when in ICU and they do not give insulin below 200 for ICU patients. Resident says they used to and patients did worse. Holly contradicts this though, saying wounds can’t heal properly with high blood sugar. Labs all say normal range is 70-99, I’ve always went with 80-120, some doctors have told me 100-150 for a diabetic.
November 13th. Overnight was uneventful. Ventilator settings are still the same. They had her Fentanyl down to 250 but overnight increased it to 350 which is still lower than a couple days ago at 400. Currently waiting on rounds. Nurse this morning tried to draw labs from the central line and unfortunately it’s not giving blood return so she tried to draw blood in Christy’s hand. Of course her veins were too small to hit even with the ultrasound machine to help.
November 14th. They attempted to turn her head so they could move her central line from one side of her neck to the other, concerned it’s a possible infection source and now, is not giving a blood return for labs. When they tried to turn her head, she quickly desaturated down into the 40s and was in very bad shape. Seems a shared concern is no longer when will she get better, but when will her body give up. For what it’s worth, a lot of the nursing staff seems genuinely concerned and upset for her. The resident mentioned the drop could have possibly been caused by a cuff leak around the tube when they tried moving her head. Now she’s flipped back on her stomach again and saturation is better, but she’s paralyzed again. Back to square one, the last 3 weeks a complete waste and setback.
November 16th. Today wasn’t a terrible day. They moved the tube 1cm down further in her throat. The theory is because the tube has been in place for so long, that the cuff at the end of the tube that seals her airway off may have slightly deformed her trachea causing the leak and her saturation dropping when they try moving her. Seems logical. Looks like that was the issue. She’s been in the 90s all day even with them lowering vent settings throughout the day. It’s now 10:45pm and they went from 100% oxygen and 18 peep down to 85% and 16 and she’s still at a saturation in the low 90s. Perfectly acceptable. Far from out of the woods, but at least she’s not going backwards again.
November 18th. Yesterday I had to leave the hospital to go home and restock my meds, meal prep, do laundry and finally see a chiropractor. They flipped Christy onto her back for a little bit around 10:30 and she did ok. Around 2:30 she didn’t seem to be tolerating it well so they flipped her back to her stomach again. She remained that way the rest of the night, over night being on 85% oxygen with saturations in the mid lower 90s. This morning they decided to flip her again and as of 12:30 her saturation is 91, though they have her back up to 100% oxygen. Let’s see how the rest of the day goes. Worth noting: Last night I received more of her medical records and spent a few hours going through them all. Nothing jumps out at me. Still doesn’t add up how she went from being perfectly fine around 5am to being extremely anxious at 6am and having to go on a ventilator at 7am because her oxygen saturation plummeted…I just don’t understand what caused her to go south so fast. Nurses note says at 6 Christy complained that the BiPAP was giving her cold air, which could cause anxiety…no more mention of this after that.
November 19th. Last night was quite emotional for me. Christy had been doing well, oxygen saturations staying in the mid-low 90s. I went to go grab something to drink from the vending machine outside the ICU and when I came back in, I noticed that her oxygen was down to 87-88 which isn’t terrible, but odd that it was fine moments before. I sat my drinks down and stood beside her hospital bed and was watching her. I noticed the usual little things like her slightly breathing over the ventilator, which would indicate she wasn’t 100% paralyzed. Not a big deal, she’s not fighting it, so why rock the boat…wait a minute…her eyebrows are moving around…that’s not supposed to happen. I said her name out loud and she stopped moving. I asked her if she could hear me, and if she could if she could move her toes. No response. I asked her if she could move her eyebrows AND SHE DID. I was blown away. I wasn’t totally sure it wasn’t just coincidence so I asked her a couple questions that would require a yes/no answer and each yes question she moved her eyebrows again. A wave of joy and happiness rushed over my entire being and I started crying and telling her how much i loved her, assuring her I’ve been here the whole time and that I miss her so much. First time in over 3 weeks I’ve actually had a visual response from talking to my wife. Sure it wasn’t verbal BUT WE TALKED TO EACH OTHER! I run and grab the nurse to tell her about it, and she said she thought she saw Christy moving her eyebrows a little while ago but didn’t put any thought into it. She comes in and also asks Christy to move her toes, nothing. Asks her to move her fingers, nothing. Asks her to “move your eyebrows like you did for your husband” and she did…even the nurse was floored. Only problem is, now we know she’s awake and aware, and knows she’s paralyzed and probably freaking out. They increased her sedative and paralytic so she’s out again. It was a beautiful moment while it lasted, but it’s a good sign for now.
Nothing really new this morning. Still on her back, saturation still in the 90s. They’re turning off the paralytic right now to see how she tolerates it. She’ll still be sedated but at least now she wont be paralyzed.
November 21st. Today is the last day Dr Preus will be the attending until after Christmas. He (respectfully) hopes he doesn’t have to see us when he comes back. Christy is holding steady. Eyes open half way, some very slight movement left/right, blinking is still a little slow. Some head and shoulder movement but that’s about it, she’s still very sedated. OH, and she just moved her fingers finally. Oxygen has been holding pretty well as well, now at 85% on the ventilator and her saturation in the low 90s. She recovers a little easier from coughing. Still a very long way to go before she’s out of here, but I’ll take it…Next concern…It’s Thanksgiving week, Caleb has his pictures Tuesday, Emma is having lasagna with my parents as well, back and forth travel with the kids a lot this week. I’m staying with Christy as much as I can this week though because Murugan is back tomorrow. I genuinely fear for her life when he’s here… I know most of Tuesday and wednesday I’ll be gone. Some of the family works Thanksgiving so plan is over weekend sometime, so I’m staying here Thursday…Please pray Murugan keeps his talons off my wife and she stays safe.
November 25th. Thanksgiving. So the past few days have been better than most. Christy is completely aware of her surroundings. She’s now moving fingers independently and hands at the wrist, both feet wiggle around a bit, very clear yes/no head movements, shoulder shrugs, lifting her arms a small amount, eyes actually moving better as well. She spent a couple days with the respirator set to spontaneous, which means it only delivers a breath when she initiates it. She’s doing the bulk of her own breathing like this which is great, breathing about 20 times a minute, and the vent set to 80% 16 peep. Complete night and day from last week.
Caleb had his newborn photos Tuesday. Holly was phenomenal as always. But here’s the best news so far….. After Caleb’s photos, we went straight to the hospital and Mommy and baby boy were finally reunited (that Christy can remember). It was a emotional time for all of us. Caleb was fussy until I laid him in her arms, then he calmed right down and fell asleep laying on mommy. It was a beautiful thing to see, after all the hospital’s put her through.
Christy wears Color Street nails and Friday her nurse noticed that she was wearing a set as she also wears them. She said she had a set of Thanksgiving strips from last year she would bring in and redo Christy’s nails for her. Her and 2 other nurses Sunday night took off all of her old nail strips and applied the new strips for her. This is way more than going above and beyond…and it meant a lot to me they would do this for her. God bless you ladies.
For what it’s worth, the nursing staff has been the best part of our time here so far, and I respect each and every one of the nurses that have taken care of Christy. Maybe I don’t say it enough, but I hope these ladies know how much I appreciate everything they do for her. It’s not their fault that those with decision making power will ‘uphold the systems values’ and treat patients like numbers and dollar signs instead of treating patients as individuals, with more personalized treatment… Yeah. Cookie cutters only work in baking. Sorry, not sorry.
November 26th. Yesterday most of the day Christy’s saturation was in the mid 80s but as the evening progressed, she kept dropping lower, eventually hitting the mid-low 70s. They decided to paralyze her again and put her back on her stomach. She’s now back in the mid 80s. As much as I hate this place and those in charge, nobody is to blame this time, I saw it all happen myself. All we can do is watch and wait and pray she turns around again.
November 29th. Looks like we are seeing the beginning of the end. Yesterday Christy’s saturation dropped and they did a chest xray. Found out she has a pneumothorax which is air stuck between the lung and lining. They put in a chest tube. All of this began around 8am. This hospital, felt it was perfectly ok to wait FOUR HOURS before contacting me! Here comes the rant…
So I have a little secret. Magee has been aware of the existence of the website and Facebook page. They sent out a mass email to the ENTIRE ICU STAFF as well as the MDs and some administration. The email originated from Brittany, don’t have last name on her, advising staff not to talk about it, comment on it, or share it and to uphold the systems values, but someone was checking it regularly. I’ve known about the email since Tuesday, but didn’t let them know.
So, you mean to tell me, that this hospital has no problem watching me and what I post/say/share, but couldn’t have the foresight to tell me my wife was crashing, FOR FOUR HOURS!!!!!??? This is BEYOND unacceptable! I asked if I should be coming back and they said they would let me know. I’m hours away from the hospital and unable to drive myself there. The hospital calls me again a few hours later to inform me Christy’s heart had stopped but they were able to restart it, and that I should consider coming back. Thank God her sister Kat was there and able to take me there. We get there and they stop us at the front desk, holding us there because “security has to escort us up”… Now my blood starts to boil. We get up to the unit and a there’s 2 people with her I don’t remember who, but I laid into them, and I made sure the level of dissatisfaction was well understood. Come to find out they shut off all sedation and giving nothing for pain…my wife has spent all day, literally over 12 hours, laying here awake and aware and most likely in a lot of pain. I quickly asked why they were off and nurses put them back on. I don’t remember much of the rest of the night after that.
This morning her SATs are up again but now it seems her kidneys are failing. It’s just a countdown to the end at this point it seems.
November 30th. Things are looking worse. Her kidneys are failing, liver function decreasing, potassium is climbing and there’s no sign of it stopping. They installed a dialysis port and will begin treatment in the morning…long shot but worth trying.
December 1st. I slept at her bedside in a chair, holding her hand all night. Her hand was cold and clammy. I haven’t seen her eyes, eyebrows or lips move all day. Things are getting rapidly worse. Her temperature which used to be a fever is now turning into hypothermia. Her face is now lifeless and her pupils are fixed wide open and dilated. She’s no longer breathing over the ventilator, it’s like she was on a paralytic again, but she wasn’t. She just lay there, still as a tree with no breeze. Her kidneys seem to be responding to the dialysis, but now her liver quit and her blood sugar is quickly dropping to dangerous levels and her blood pressure keeps dropping. This is bad. As the hours wind down, her temperature, heart rate, and blood pressure keep dropping. They give her two IV meds to bring her blood pressure back up, but it’s just a bandaid for what we now realize will be a permanent problem. She’s already gone. All that’s left is a heartbeat, the only organ that didn’t completely give up already. The meds are maxed out now and can’t go any higher, her heart rate and blood pressure are continuing to fall. 70 beats becomes 60, becomes 50, becomes 40. After this, it comes much quicker. We all say our goodbyes and Holly, Kat, Jayme (her oldest daughter) and I all are holding her hand, shoulder, etc as her heart rate slows below 20 beats per minute until it just stops. It is now 8:09pm and my wife is now gone for good. A life wasted that didn’t need to be, all because of a health system and doctors/administrators that care more about profits than actually taking care of people. Let this be a lesson to you all. NEVER trust your loved ones to ANY UPMC facility if you value their lives, and for God’s sake, don’t ever go to Magee Women’s Hospital of Pittsburgh, PA.
In closing, on behalf of my family, I would like to personally thank all of the following people for giving my wife every chance they could with the limited tools they were given. Macey, Ricki, Andrea, Jenna, Jenny, Cole, Eponine, Amber, Marissa, Bill(RT), Denny(RT), Bill(RT director), Dr White, Dr Preus, and the rest of the nurses who’s names I regretfully can’t remember right now. God bless you all, and thank you for every last moment you gave me with my wife.
Christy, the love of my life, mother of my 3 children, and my best friend. We didn’t get nearly enough time together. What was supposed to be a lifetime, was barely over 6 years. You are my rock, my life, my world, and my everything. I can’t imagine life without you but I guess I don’t have the choice anymore. I’m going to miss you so much. I may have failed to protect you from this, and I am so sorry for that, but you have my word, your children WILL know you and WILL remember you. I am so thankful that you had the opportunity to finally see and hold Caleb, he’s such a beautiful baby boy and I hope you have some peace knowing he still remembers you even tough this prison took your time with him away. I will always remember you, always love you and always miss you. Till death do us part just ain’t enough. Until we meet again beautiful, I love you, so much. You will forever be my always.
Christy Leigh Cresto, 33 of Export, passed away Wednesday, December 1, 2021 at Magee Women’s Hospital in Oakland, PA.
Born January 30, 1988 in Pittsburgh, PA, she was the daughter of Holly S, (Scott) Daum and the late Harold H. Daum, II
Christy was a housewife and mother. She was involved with the PTO at Franklin Regional Elementary School and competitive cheerleading. Christy enjoyed gymnastics, horses, crafts, interior decorating, writing, cooking, baking cookies and most of all she was devoted to her family with all her Love.
Filter By Category
Age: 67
Location: MT
Admitted: 10/30/2021
To: Providence St. Patrick’s Hospital, Missoula, MT
Murdered: 11/13/2021
Martin William Maclay

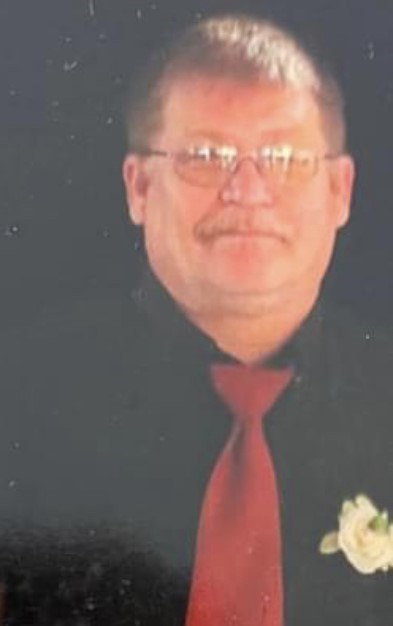
Age: 62
Location: TX
Admitted: 10/23/2020
To: Medical Arts Lamesa Texas than Covenant Lubbock Texas.
Murdered: 11/13/2020
Lawny Dale Cannon II

Age: 41
Location: AR
Admitted: 09/22/2021
To: Baptist Health
Crystal Marie Alonzo

Age: 63
Location: TX
Admitted: 01/30/2022
To: ST David’s Austin
Murdered: 03/01/2022
Joe Bradshaw

Age: 70
Location: CA
Admitted: 12/30/2020
To: Kaiser
Murdered: 01/08/2021
John Grijalva

Age: 82
Location: MT
Admitted: 10/10/2022
To: St.Peters , Helena,Mt
Murdered: 10/26/2022
Shirley Herrin

Age: 42
Location: GA
Admitted: 08/31/2021
To: Floyd Medical Hospital, Rome, GA (now Atrium Health Floyd)
Murdered: 09/07/2021
Johnny Glenn Moore, Jr.

Age: 87
Location: NV
Admitted: 10/02/2021
To: Henderson Hospital
Murdered: 10/18/2021
Relda Grady

Age: 57
Location: TX
Admitted: 07/01/2021
To: Mansfield Methodist Medical Center
Murdered: 08/11/2021
Michael Peterson

Age: 68
Location: FL
Admitted: 09/04/2021
To: Voca Regional Hospital
Murdered: 10/02/2021
Curtis K. Elrod

Age: 64
Location: TX
Admitted: 08/28/2021
To: Gainesville Medical Center
Murdered: 09/16/2021
Andy Serna

Age: 78
Location: CA
Admitted: 09/01/2021
To: Saint Agnes Medical Center
Murdered: 10/02/2021
Josephine Hutchens

Age: 55
Location: FL
Admitted: 07/03/2021
To: Advent
Cheryl Holley

Age: 64
Location: UT
Admitted: 10/22/2021
To: St Johns
Murdered: 01/07/2022
Father Ubald Rugirangoga

Age: 46
Location: NC
Admitted: 11/30/2021
To: Atrium Health Wake Forest Baptist Medical Center
John W. Taylor

Age: 24
Location: NY
Admitted: 11/10/2021
To: Columbia Memorial Hospital and Westchester Medical Center
Murdered: 12/08/2021
Jeremy Budik
Age: 59
Location: MO
Admitted: 08/06/2021
To: Bothwell in Sedalia/Truman VA Hospital in Columbia Mo
Murdered: 08/26/2021
LeRoy Hill

Age: 48
Location: FL
Trinna Patterson

Age: 49
Location: LA
Admitted: 07/26/2021
To: Thibodeaux Regional Medical Center
Murdered: 08/28/2021
Pauline "Bugzie" Barrilleaux

Location: FL
Admitted: 12/27/2021
To: Morton Plant Bayside Hospital Group
John C Keane

Age: 60
Location: GA
Admitted: 08/21/2021
To: Northside Hospital Forsyth
Murdered: 09/14/2021
Robert Coleman

Age: 46
Location: FL
Admitted: 08/12/2021
To: Lakeland Regional Health
Murdered: 08/24/2021
James D Thrift Jr (“Donny”)

Age: 68
Location: MO
Admitted: 07/17/2021
To: Liberty Hospital
Murdered: 07/28/2021
James Freed

Age: 62
Location: MI
Admitted: 04/26/2021
To: Henry Ford Hospital
Murdered: 05/04/2021
Francesco Todaro
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.