
Injured by the Shot
Age: 48
Location: LA
Became sick: 08/01/2022
First sought care: 08/01/2022
Kim Michael Rivet



This all started on October 31, 2021 when Jason told me he had a sore throat. No other symptoms were present. On 11/06 Jason went to the ER at Ashe Memorial for shortness of breath. He tested positive for Covid and they gave him one dose of Remdesivir without his consent. This is AFTER he stated multiple times that he wouldn’t be taking it. He had bloodwork taken and I requested a D Dimer. It came back at 428. He was admitted after an x-ray showed bilateral pneumonia.
At 11:51 on 11/07 he texted me letting me know that they were going to discharge him, even though the D Dimer they took at 06:53 was 564. I then requested a CT Angio be done to check for Pulmonary Emboli before he was discharged since his levels went up, even after a 40mg sub-Q injection of Lovenox. Scan showed moderate burden of diffuse multifocal pulmonary opacities compatible with atypical pneumonia. He was then discharged. I brought him home and he slept all day and night, only to get up to go to the bathroom which exhausted him.
I woke him up on November 9th to check his oxygen levels. He had severe worsening shortness of breath along with blue tinged lips and incoherence. His oxygen was 58%. I got the kids into the car and helped get him into the car, then rushed him back to Ashe Memorial. I ran inside to tell the triage nurse how low his oxygen was and that he was confused and lethargic. They would come out over 5 minutes later with a wheelchair. There was no sense of urgency at this time. Once he went through those doors I would not hear from him without a fight. Once they got him in at 1035 he was satting at 61% so they put on nasal cannula and he got up to 85%.
It wasn’t until 1239 that they put him on CPAP. I kept texting him but got no answer. I then called the hospital to get an update and to talk to him and his nurse told me that I could not talk to him. I demanded that he be put on the phone and she said no. I told her that I am getting in the car with our kids and that I would be there in less than 10 minutes. I arrived and was met at the ambulance bay by his nurse, along with a security guard “for my safety”. I facetimed his work phone which I then handed to his nurse to take into his room. He looked awful. I was able to get him to make me Healthcare Power of Attorney and told him I would advocate for him.
He would go back in for a repeat CTA, and at 1504 radiology stated that there was significant worsening of bilateral multifocal pneumonia. They wanted to admit him but had no available beds. They called surrounding hospitals but the majority consensus was that he would need to be intubated before they would accept him. They stated in his chart that he was a DNI/DNR. He would never sign a DNI/DNR, he only asked that they wouldn’t intubate him unless he wasn’t able to keep his oxygen levels up on his own. They have not given him any blood thinners yet. They finally drew a D Dimer at 0748 on 11/10 and it was 2060. After 30 hours in the emergency room, he was finally admitted to the monitored bed unit on 11/10. He was given one dose of Lovenox 40mg that evening.
On 11/11 at 0413 his D Dimer was 1770. I called the hospital again to get them to do an ultrasound of his legs to check for DVT since his D Dimer was so high. At 0911 on 11/11 the ultrasound was performed with no findings. According to his records, no blood thinners were given on 11/11.
On 11/12 at 0817 his D Dimer was 4250.His Lovenox dosage was increased to 1mg/kg. He was given 130mg of Lovenox. I requested a repeat CTA be done given the significant jump to his D Dimer. After going back and forth with the doctor, she reluctantly agreed. CTA was done at 1233 and showed small bilateral pulmonary effusions along with severe bilateral lung infiltrates. I called the hospital and asked to speak to the patient advocate. She said that I would not be able to see him. This was an unacceptable answer. I went to the hospital and demanded to speak to whoever was in charge. I told her that I was not leaving until I was able to see him. She agreed to one 20 minute visit once a day.
Thankfully his nurse at the time was more gracious than the hospital and allowed me to stay for a few hours. When I walked into his room we made eye contact. There was instant relief along with tears. He laid his head on my chest and was able to finally relax since he had entered the er. He was able to tell me that they are never in his room. He was scared and didn’t want me to ever leave him alone. After a few hours of rubbing his neck and shoulders I was told that it was time to go. I asked to speak to his doctor about his care or lack thereof. She seemed irritated that I was not satisfied with how he was being treated. After about 20 minutes of going back and forth, we agreed on is healthcare plan from here on out. He was given a second dose of Lovenox 170mg.
On 11/13 his D Dimer was 4820 at 0330. CTA was repeated and showed that bilateral lung infiltrates were worse. Doctors note states that due to an absence of demonstratable PE, she was reducing his Lovenox to .5mg/kg. He was given 85mg of Lovenox. I arrived shortly before noon. He told me that they had not given him any meds today. He rang the nurse around 0745 to get help to the toilet but no one answered. They just sat at the nurses station across from his room and laughed/talked. He ended up making it to the toilet himself, almost removing the CPAP in the process due to the tangled tubes/cords. I spent the next 6 hours rubbing his neck, shoulders, legs, and feet. When I left, he was getting very anxious. He said that no one listens when I am not there. I asked the nurse if they could give him something small for the anxiety he was having, as it was increasing his heart and respiration rates. She said that she would talk to the doctor. They gave him 1mg Klonopin, 1mg Ativan, and 20mg Prozac.
On 11/14 at 0513 D Dimer was <5000. 5000 is the highest they can detect. No Lovenox was given. No CTA was performed. He called me at 0537 but I couldn’t hear him due to the CPAP. I texted him back and asked what’s wrong. He texted “answer”. I then asked if he was calling me because he wanted me to come up to the hospital. He answered “yes”. I let him know that I would leave as soon as my mom (who drove 1000 on Thursday to watch my kids so I could fight for Jason) wakes up. I also asked if he was ok. He answered “sort of” at 0600. At 0719 he texted “Where did you go?”. I told him that I wasn’t there yet. His mental state was rapidly declining so I rushed up to his room immediately. When I arrived, he did not look well at all. His oxygen levels were low for him being on CPAP 100%.
I told his nurse that I wanted to talk to the doctor immediately. She never came. After a bit, he wanted to switch to the chair because he was very uncomfortable. I helped him up and he collapsed into my arms, gasping for each breath. I got him into the chair and he ripped off his CPAP mask saying that he couldn’t breathe. I pushed the call button and told them to get into the room now! They slowly made their way in. I was able to get the CPAP mask over his nose and mouth and pressed firmly until respiratory came in and got the mask secured. Dr. Sullivan finally came in and told him that he needed to be intubated. He nodded yes. She said again Jason do you want to be intubated. He looked at me like didn’t she already say that? While he was nodding yes, I yelled DO IT! They started getting everything ready. Slowly, another doctor came in.
Precious minutes passed before they finally moved him back onto the bed. By this time his skin was grey. His lips blue. His eyes scared and distant. They gave him 100mg of Versed once he was in position and bagged him. The doctor said “push rocks and lets roll”. 250mcg of Fentanyl and 200mg Succs was given and then he intubated him. I was getting worried because his pulse was in the 30’s. The doctor said it would go back up, just to give it time. I said “He doesn’t have time!”. They finally gave him 1mg Epinephrine with no improvement. After a few more minutes of waiting, they finally called a code blue. Compressions were started and I was led out and seated at the nurses station across from his room where I could see everything. I then called his parents, my pastor, and my mom to let them know what was going on. None of them could believe it.
I stayed on the phone with my mom on speaker so she could hear what was going on. After about 15 minutes, Dr. Sullivan came to me and said it wasn’t looking good and that he probably wasn’t going to make it. I asked her if they were going to shock him. She stated that he doesn’t have the right rhythm to shock and that doing so would cause more damage than good. I said “more good than dying?”. She shrugged her shoulders, said per ACLS protocol they could only do CPR for 30 minutes total and not a minute extra. She then walked back into the room. ACLS protocol also states that 1mg Epinephrine be given EVERY 3-5 minutes during compressions.
Dr. Sullivan states in her notes that additional rounds of Epinephrine were administered as documented. The detailed billing statement only shows 1mg was given, TOTAL! I looked into his room and saw them stop. Dr. Sullivan approached me, shrugged her shoulders, said sorry with what could only be considered a sarcastic grin, and walked away. His nurse came to me and embraced me saying that he was gone. I lost it. I called his parents who cried out with intense grief. Then called my mom who had to keep it together for my kids. After I called my Pastor who ran into the church, said no church today Jason just passed away, prayed together, then headed toward the hospital.
After a few minutes, I was able to muster up the strength to stand up and go to his bedside. I sat next to him, wailing and holding his hand. Pastor arrived and prayed with me and waited until his parents got there. I had them extubate him as I didn’t want them to see him like that. When they arrived all I could hear was his little brother moaning and crying and his mom saying “Lord no, not my baby”. His dad then came in crying and rubbing Jason’s feet along with Chrissy, his little brothers wife, who embraced me and kept repeating “I am so sorry”. The patient advocate came in and spoke about getting a funeral home arranged. I requested that an autopsy be done and the Medical Examiner at Ashe Memorial refused. His parents would pay a large amount for a private party to carry out the autopsy. Dr. Sullivan never came back, despite what is written in her reports.
Now I had to leave the love of my life and go home to our kids. I had to tell them that their father was in heaven now. Rob, Jason’s father, drove me home. The whole way I’m trying to find the words to tell the kids. Once I entered the house, I told my kids to come sit on the couch with me. Pastor and his wife were there for support. I told them that daddy was in heaven and wasn’t in any pain anymore. Our 10 year old lost it, crying out that he couldn’t be gone. Our 8 year old wasn’t comprehending it, so more questions were answered before she understood and cried out. Our 5 year old son asked when daddy was coming back from heaven. I told him that he wasn’t and that is when he started crying.
Autopsy revealed that he had massive showers of pulmonary emboli in both lungs. He stated that there were so many pulmonary emboli that he lost count. He also had dilated cardiomyopathy which was never stated in any of the radiologists’ reports. He also stated that in Jason’s case, had he been given the correct meds he would have made it through. It would have been a long road, but he would have made it. Dr. Sullivan wouldn’t sign the death certificate unless the cause of death was Covid. The pathologist refused to put it as the primary but we had to settle as secondary COD in order to get the death certificate.
When it was time for the private viewing, I told my kids that they at least needed to see him. They walked in and stopped short of the casket. Abigail(10) just stared and cried, Haley(8) cried, and Samuel(5) touched him then jumped back and asked why he was so cold. Family came and paid their respects then it was time to go. One by one my kids stepped up to say goodbye. Samuel said “I love you Daddy” and rubbed his head. Haley said “I’m going to miss you Daddy” and placed her hand on his. Abigail needed some time alone with him. She finally said “I love you Daddy” then fell into my arms.
I led them out to family then I said my goodbyes. The next day we had the funeral. His grandfather was able to privately say his goodbyes as he wasn’t able to drive at night for the viewing. I married Jason on November 20, 2010 and said goodbye to his body on November 20, 2021, our 11 year anniversary. I got to love him for 10 years 51 weeks and 6 days.
What this hospital did to him is disgusting. Nobody should be treated that way. Doctors and nurses take a hypocritic oath to First, DO NO HARM. Yet they killed him. They took my husband, the father of my 3 kids, a son, a brother, an uncle, a cousin, a friend, the breadwinner, my rock, my first love. It is unacceptable and I WILL have justice for Jason.
Filter By Category

Age: 48
Location: LA
Became sick: 08/01/2022
First sought care: 08/01/2022
Kim Michael Rivet

Age: 67
Location: MN
Became sick: 11/20/2021
First sought care: 11/27/2021
Admitted: 11/29/2021
To: Mercy Hospital
Murdered: 12/12/2021
Ray Evangelista

Age: 68
Location: TN
Became sick: 01/22/2022
First sought care: 01/22/2022
Admitted: 01/24/2022
To: Baroness Erlanger, Life Care Center of East Ridge, and Sisken Hospital
Murdered: 02/10/2022
Mary E. Reiter

Age: 51
Location: NY
Became sick: 01/18/2022
First sought care: 01/25/2022
Admitted: 01/25/2022
To: St. John’s Episcopal
Murdered: 02/13/2022
Jamell Jones

Age: 30
Location: OH
Became sick: 08/03/2021
First sought care: 08/03/2021
Admitted: 08/28/2022
To: The Cleveland Clinic Main Campus -Cleveland Ohio
Jillian M. Friedman

Age: 62
Location: TX
Became sick: 10/16/2020
First sought care: 10/20/2020
Admitted: 10/23/2020
To: Medical Arts Lamesa Texas than Covenant Lubbock Texas.
Murdered: 11/13/2020
Lawny Dale Cannon II

Age: 62
Location: CO
Became sick: 10/12/2021
First sought care: 10/17/2021
Admitted: 10/17/2022
To: Sam- Saint Anthony / Andrew - Lutheran Medical
Murdered: 11/05/2021
Samuel Miller and Andrew Miller
Age: 78
Location: GA
Became sick: 12/15/2021
First sought care: 12/22/2021
Admitted: 01/01/2022
To: Newnan Hospital
Murdered: 01/17/2022
James

Age: 77
Location: FL
Became sick: 08/07/2021
First sought care: 08/10/2021
Admitted: 08/10/2021
To: Horizon West Orlando; Health Central (died there)
Murdered: 08/20/2021
Crisantemo T. Concepcion

Age: 48
Location: IL
Became sick: 11/29/2021
First sought care: 12/06/2021
Admitted: 12/27/2021
To: Northwestern Medicine Kishwaukee Hospital
Murdered: 02/28/2022
Michelle Bruno

Age: 77
Location: OH
Became sick: 07/29/2021
First sought care: 07/31/2021
Admitted: 07/31/2021
To: Ohio Health Mansfield
Murdered: 12/23/2021
James "Jim" Miller

Age: 74
Location: TX
Became sick: 03/05/2021
First sought care: 03/07/2021
Admitted: 03/07/2021
To: Baylor Scott and White
Murdered: 03/14/2021
Constantine Kotsanis

Age: 60
Location: WI
Became sick: 11/02/2021
First sought care: 11/05/2021
Admitted: 11/05/2021
To: Aurora Bay Care
Jane Krueger

Age: 70
Location: TX
Became sick: 08/19/2021
First sought care: 08/19/2021
Admitted: 08/19/2021
To: Texas Health Harris Methodist Hospital
Murdered: 09/01/2021
Tennis Ingebretson

Age: 65
Location: WA
Became sick: 08/05/2021
First sought care: 08/11/2011
Admitted: 08/11/2021
To: Kadlec Regional Medical Center
Murdered: 09/04/2021
Shannon Michael Washburn

Age: 55
Location: FL
Became sick: 07/02/2021
First sought care: 07/03/2021
Admitted: 07/03/2021
To: Advent
Cheryl Holley

Age: 54
Location: CA
Became sick: 01/01/2022
First sought care: 01/03/2022
Admitted: 01/09/2022
To: Beverly Community Hospital
Murdered: 02/05/2022
Larry Gonzales

Age: 64
Location: PA
Became sick: 09/06/2021
First sought care: 09/11/2021
Admitted: 09/11/2021
To: UPMC
Murdered: 09/12/2021
Mary Conroy

Age: 56
Location: WY
Became sick: 09/30/2021
First sought care: 10/07/2021
Admitted: 10/16/2021
To: Wyoming Medical Center
Murdered: 11/03/2021
Richard “Zak” Szekely

Age: 87
Location: PA
Became sick: 11/09/2021
First sought care: 11/09/2021
Admitted: 11/08/2021
To: Doyelstown
Murdered: 11/20/2021
Inge Kornfeld

Age: 80
Location: GA
Became sick: 12/24/2021
First sought care: 12/28/2021
Admitted: 12/30/2021
To: St Mary's Athens GA
Murdered: 01/11/2022
Gary Phillips

Age: 59
Location: OK
Became sick: 09/07/2021
First sought care: 09/17/2021
Admitted: 09/22/2021
To: Oklahoma City VA hospital
Murdered: 09/26/2021
Michael Lee Hood

Age: 44
Location: KY
Became sick: 08/23/2021
First sought care: 09/01/2021
Admitted: 09/05/2021
To: Mercy Health Lourdes Paducah
Murdered: 10/16/2021
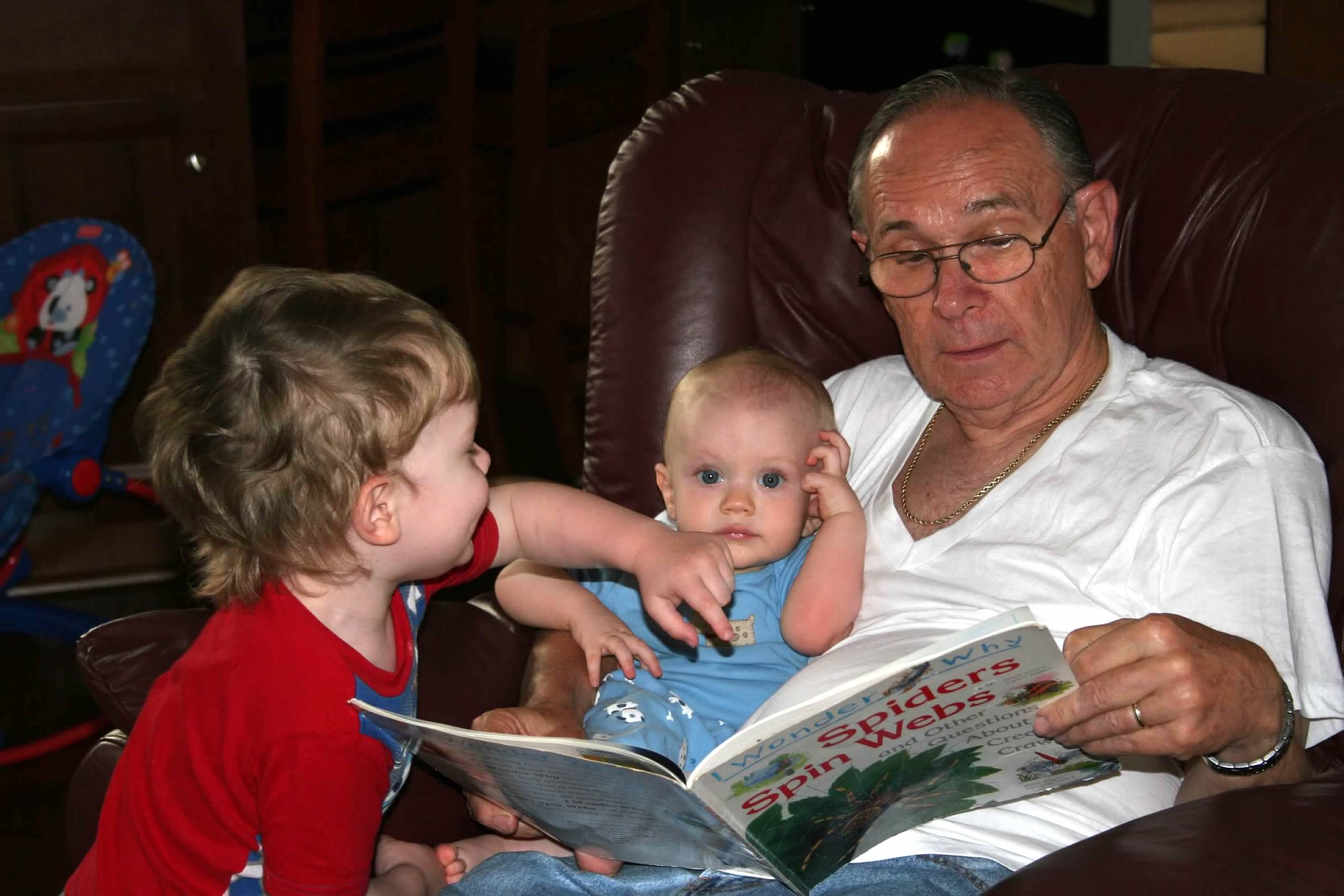
Jason Parks
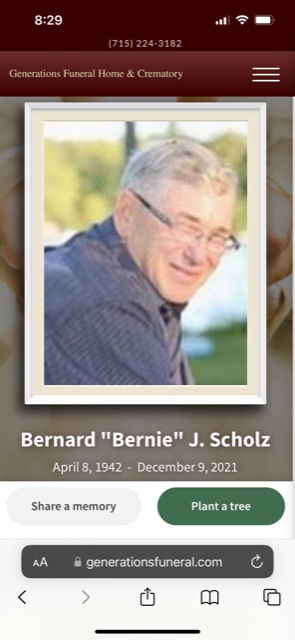
Age: 79
Location: WI
Became sick: 11/20/2021
First sought care: 11/30/2021
Admitted: 12/03/2021
To: Aspirus Medford Hospital
Murdered: 12/09/2021
Bernard Joseph Scholz
These are just a few of the cases archived by our COVID-19 Humanity Betrayal Memory Project, and there are more being reported by survivors and families of victims every day. If you would like to help with this project, please consider becoming part of the Task Citizens Force Against Instutional Capture And Crimes Against Humanity, a FormerFedsGroup Freedom Foundation mission.